Table of Contents >> Show >> Hide
- What “impending doom” actually means
- Why it feels so real: the brain-body alarm system
- Mental health-related causes (common and treatable)
- Medical causes that can feel like doom (and when it’s urgent)
- When to treat it as an emergency
- How doctors evaluate a “doom feeling”
- What to do in the moment (practical, non-cringey steps)
- Long-term strategies that actually move the needle
- FAQ: quick answers to common questions
- Conclusion
- Experiences people report (500+ words of real-life feel)
A “feeling of impending doom” sounds like a dramatic line from a superhero movie… until it happens to you in real life.
Suddenly your brain is convinced something terrible is about to happenno obvious reason, no clear threat, just a heavy,
urgent certainty that screams danger.
Here’s the tricky part: this feeling can show up during very treatable anxiety conditions and during certain medical
emergencies. That’s why it deserves respect, not embarrassment. The goal of this guide is to help you understand what it means,
why it happens, how to tell when it might be urgent, and what to do nextwithout spiraling into “WebMD Olympics.”
What “impending doom” actually means
Clinicians use “sense of impending doom” to describe an intense, distressing belief that something catastrophic is about to occur,
often paired with fear of death, fear of losing control, or a powerful “something is wrong” sensation. It’s not the same as ordinary
worry. Regular worry tends to sound like: “What if?” Impending doom tends to sound like: “It’s happening.”
The feeling can be emotional (terror, dread), physical (tight chest, nausea, shakiness), cognitive (racing thoughts),
or all three at once. It may last minutes, come in waves, or hover like a storm cloud that won’t move along.
Why it feels so real: the brain-body alarm system
Your body has a built-in alarm system designed to keep you alive. When it detects potential danger (real or perceived),
it can flip on the “fight-or-flight” response: faster heart rate, faster breathing, sweating, trembling, and hyper-alertness.
These sensations are uncomfortableand your brain hates mystery discomfort.
So the brain does what brains do best: it tries to explain the signals. If your heart is pounding, your breathing feels weird,
or your body suddenly surges with adrenaline, your mind may decide: “This must be a big threat.” That interpretation can
instantly create dreadand dread can intensify the body sensations. Congratulations, you’ve discovered the world’s least fun
feedback loop.
Sometimes that loop is driven primarily by anxiety. Other times, the body is signaling a medical problem that needs urgent care.
The sensation itself is real either way. The question is what’s powering it.
Mental health-related causes (common and treatable)
Panic attacks and panic disorder
Panic attacks are sudden surges of intense fear that can include a sense of impending doom, fear of dying, and physical symptoms
like rapid heartbeat, sweating, trembling, chest discomfort, choking sensations, dizziness, and tingling. Many people truly believe
they’re having a heart attack, “going crazy,” or about to pass outeven though panic attacks themselves are not usually dangerous.
Panic disorder is diagnosed when panic attacks are recurrent and lead to ongoing worry about future attacks or avoidance of places
and situations. The avoidance can quietly shrink someone’s life: fewer outings, fewer social plans, fewer “normal” days, all because
the brain is trying to prevent another terrifying episode.
Generalized anxiety, chronic stress, and “doom scrolling”
Generalized anxiety can create a persistent sense that something bad is coming, even when life is calm on paper. Chronic stress can
keep your nervous system running hotso your baseline starts to feel like “mild emergency.” Add caffeine, dehydration, poor sleep,
and constant notifications, and your body becomes a highly talented disaster narrator.
In the modern era, doom can also be socially contagious. If your feed is a non-stop highlight reel of catastrophe, your brain may
treat the world as permanently unsafethen it starts scanning your body for proof.
Sleep anxiety (and the 2 a.m. spiral)
Anxiety doesn’t just make it hard to sleep; it can make bedtime feel like an audition you’re failing. People with sleep anxiety may
feel restless, irritable, overwhelmed, and stuck with a “something bad is about to happen” vibe when the lights go out.
The body sensations of anxietyfast heart rate, rapid breathing, tense musclescan amplify the dread.
Trauma-related symptoms and hypervigilance
After trauma, the nervous system may stay on alert even when you’re safe. A sound, smell, or situation can trigger a body memory:
your heart jumps, your breathing changes, and suddenly you feel threatened. The “impending doom” feeling can be the brain’s attempt
to protect youmisfiring because it’s learned to expect danger.
Substances, stimulants, and withdrawal
Stimulants (including high-dose caffeine or certain ADHD medications) can increase jitteriness and heart racing. Some decongestants,
nicotine, energy drinks, and recreational substances can also provoke anxiety-like symptoms. Withdrawal from alcohol or other
substances can cause intense anxiety, agitation, and a sense that something is very wrong.
If the doom feeling consistently shows up after a specific drink, supplement, medication change, or late-night energy drink “for science,”
that pattern is useful information to share with a clinician.
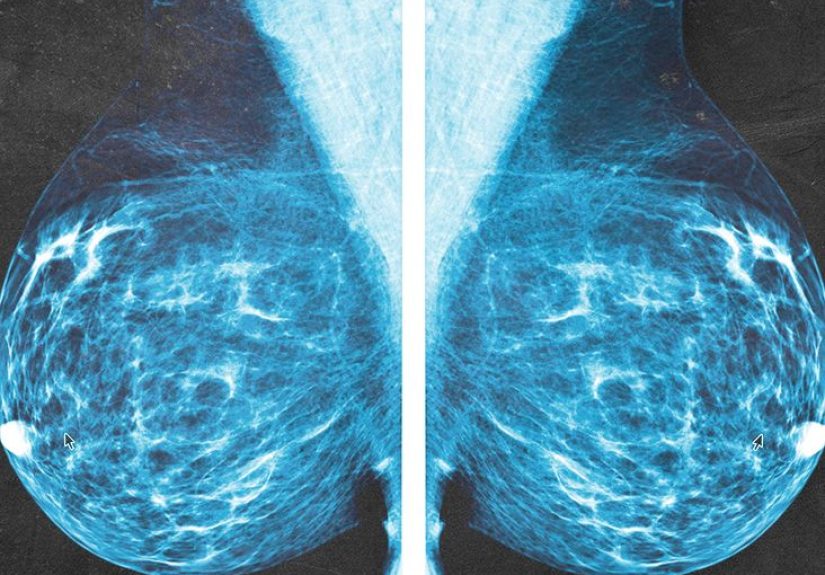
Medical causes that can feel like doom (and when it’s urgent)
A sense of impending doom can occur in medical situations where the body is under serious stressespecially when breathing,
circulation, or the immune system is involved. The feeling may appear early, even before other symptoms are obvious.
Anaphylaxis (severe allergic reaction)
Anaphylaxis is a life-threatening allergic reaction that can escalate quickly. Along with hives, swelling, breathing trouble,
throat tightness, vomiting, dizziness, or low blood pressure, some people report a sudden “sense of doom” or intense anxiety.
Because timing matters, this is an emergency.
Seek emergency care immediately if impending doom comes with trouble breathing, throat swelling, widespread hives,
fainting, or rapid worsening after a possible allergen exposure (foods, medications, insect stings, latex, etc.).
Heart attack
Heart attacks can present with chest pressure or pain, pain in the arm/back/neck/jaw, shortness of breath, sweating,
lightheadednessand sometimes anxiety or a sense of doom. Symptoms vary by person, and not everyone experiences classic crushing
chest pain.
Call emergency services right away if impending doom shows up with chest discomfort, shortness of breath, fainting,
or pain spreading to the jaw/arm/backespecially if it’s new, intense, or getting worse.
Pulmonary embolism (blood clot in the lung)
A pulmonary embolism (PE) occurs when a clot blocks blood flow in the lungs. Symptoms can include sudden shortness of breath,
chest pain (often worse with deep breathing), rapid heart rate, cough (sometimes with blood), dizziness or faintingand sometimes
a strong feeling of anxiety or dread.
PE is an emergency. If doom appears with sudden breathing difficulty, chest pain, fainting, or coughing blood, seek immediate care.
Seizures and seizure “auras”
Some focal seizures (especially temporal lobe seizures) can begin with an auraa warning sensationsuch as sudden fear, déjà vu,
stomach rising sensations, or a sense of doom. Not everyone has auras, and not everyone remembers them, but when this symptom
is new or paired with confusion, unusual sensations, or episodes of “lost time,” it’s worth medical evaluation.
Thyroid problems (especially hyperthyroidism)
An overactive thyroid can cause symptoms like fast heart rate, tremor, sweating, and anxiety. When your body is revved up,
your brain may interpret the signals as dangerleading to a doom feeling. If you have persistent palpitations, weight changes,
heat intolerance, tremor, or new anxiety that doesn’t match your life circumstances, ask a clinician about thyroid testing.
Rare adrenaline surges (pheochromocytoma)
A pheochromocytoma is a rare tumor of the adrenal gland that can cause “spells” of pounding heartbeat, sweating, headaches,
high blood pressure, and anxietyor even a sense of doom. Rare doesn’t mean “ignore it,” but it does mean you shouldn’t panic-scroll
yourself into a diagnosis. The key clue is repeated, dramatic episodes with strong physical surges.
When to treat it as an emergency
Use this as a safety checklist. If the feeling of impending doom is sudden and intense and comes with any of the following,
seek emergency care (in the U.S., call 911; elsewhere, call your local emergency number):
- Chest pain, chest pressure, or pain spreading to the arm, jaw, neck, or back
- Shortness of breath, wheezing, or throat tightness
- Fainting, severe dizziness, or new confusion
- Widespread hives, facial/lip/tongue swelling, or rapid allergic symptoms
- Coughing up blood or sudden one-sided leg swelling/pain with breathing symptoms
- New seizure symptoms, “lost time,” or sudden neurological changes
If you’re unsure, it’s better to be checked and reassured than to “tough it out” and hope your nervous system is just being dramatic.
Your body doesn’t hand out this feeling like a party favor.
How doctors evaluate a “doom feeling”
Clinicians usually start with context: when it began, how long it lasts, what triggers it, and what physical symptoms appear alongside it.
Depending on your symptoms and risk factors, evaluation may include:
- Vital signs (heart rate, blood pressure, oxygen level, temperature)
- Heart checks (exam, ECG/EKG, sometimes blood tests)
- Breathing/lung evaluation (oxygen, imaging if needed)
- Allergy history and emergency treatment review if anaphylaxis is suspected
- Basic labs (thyroid tests, blood sugar, anemia checks) when appropriate
- Mental health screening for panic disorder/anxiety when medical emergencies are ruled out
This is not “all in your head” versus “all in your body.” Anxiety lives in the body, too. A good evaluation respects both.
What to do in the moment (practical, non-cringey steps)
Step 1: Check for red flags first
Before you try to breathe it away, do a quick scan: chest pain, severe shortness of breath, fainting, swelling/hives, confusion,
or neurological symptoms? If yes: emergency care. If no: move to calming your nervous system.
Step 2: Label it (yes, it helps)
Try: “This is a surge of alarm. My body is acting like it’s in danger.” Naming it can reduce the brain’s urge to invent a catastrophic story.
Step 3: Slow the exhale
You don’t have to breathe perfectly. The goal is a slightly longer exhale than inhale. For example: inhale gently through your nose,
then exhale slowly through pursed lips. Repeat for a couple minutes. Longer exhales nudge the body toward “safe mode.”
Step 4: Ground in the physical world
Use your senses to prove to your brain that you’re here, now, and okay. Pick three things you can see. Two things you can feel
(feet on the floor, chair supporting you). One thing you can hear. This interrupts the doom narrative with reality data.
Step 5: Reduce fuel, not feelings
If caffeine, sleep deprivation, dehydration, or stress is the likely driver, focus on basics: water, a small snack, stepping outside
for fresh air, and a short walk. You’re not “curing” anxiety; you’re removing the stuff that makes your nervous system twitchy.
Long-term strategies that actually move the needle
Learn your pattern (your body leaves clues)
Keep a simple log for two weeks: when it happens, what you were doing, what you ate/drank, sleep, stress level, and symptoms.
Patterns often show up: “only after energy drinks,” “only when I’m overtired,” “only in crowded stores,” or “random, plus palpitations.”
That information helps clinicians make better decisions.
Therapy (especially CBT) for panic/anxiety cycles
Cognitive Behavioral Therapy (CBT) is commonly used for panic disorder and anxiety because it targets the fear-body-feedback loop.
It helps you reinterpret physical sensations, reduce avoidance, and regain confidence in your ability to ride out uncomfortable waves.
Medication (when appropriate)
Some people benefit from medicationoften SSRIs/SNRIs for panic disorder or anxiety, and sometimes short-term options depending on
individual circumstances. For certain physical causes, treating the underlying condition (like thyroid issues) can significantly reduce
the doom feeling. Always discuss risks and benefits with a licensed clinician.
Sleep, movement, and “nervous system maintenance”
Regular sleep, consistent meals, moderate movement, and stress management aren’t glamorous, but they are powerful. Think of it as
keeping your internal smoke detector from going off every time you make toast.
FAQ: quick answers to common questions
Can a feeling of impending doom happen for “no reason”?
It can feel like “no reason,” but there’s usually a driverpanic physiology, chronic stress, stimulant effects, sleep loss, or a medical condition.
Sometimes the trigger is subtle (like shallow breathing or a minor heart rhythm change) and your brain fills in the blanks with doom.
Is it always anxiety?
No. It’s often anxiety-related, but it can also appear with medical emergencies like anaphylaxis, heart attack, pulmonary embolism,
or seizure activity. New, severe, or unusual episodesespecially with red-flag symptomsshould be evaluated urgently.
How do I tell the difference between panic and something serious?
You can’t always tell based on feelings alone because symptoms overlap. If it’s your first episode, it’s unusually intense,
it includes chest pain, fainting, breathing trouble, swelling/hives, confusion, or neurological symptomstreat it as urgent.
If you’ve had panic attacks before and this episode matches your pattern, you can use your coping plan while still checking in
with a clinician for ongoing care.
Conclusion
A feeling of impending doom is one of the most unsettling sensations the human nervous system can produce. It may be the signature
of a panic surge, the echo of chronic stress, a trauma-driven alarm, orless commonlya warning sign of a serious medical issue.
The smartest approach is balanced: don’t dismiss it, don’t catastrophize it, and don’t try to “win” against it with willpower.
If it’s new, severe, or paired with red-flag symptoms, seek emergency care. If it’s recurring and disruptive, get evaluated and build a plan.
With the right support, most people can dramatically reduce these episodes and get their lives back from the doom soundtrack.
Experiences people report (500+ words of real-life feel)
Because “impending doom” is such a dramatic phrase, people often assume it must be rare or exaggerated. In reality, many describe it in
surprisingly similar wayslike the brain is delivering a push notification that says: Emergency. Unknown. Act now.
Below are examples of how people commonly experience it. These are not diagnosesjust relatable snapshots that can help you recognize
patterns and communicate clearly to a healthcare professional.
The “I’m dying… I’m definitely dying” panic surge
One of the most common experiences is a sudden wave of fear that feels physically unstoppable. A person might be sitting in class,
walking through a store, or scrolling on their phone when their heart suddenly starts pounding. Breathing feels “off,” like they can’t
get a satisfying breath. Their hands might tingle, their face feels hot, and the brain jumps to the worst conclusion:
“This is it. Something is terribly wrong.”
What makes it so convincing is how fast it arrives. There’s no warm-up. The mind then tries to solve the “mystery” of the body sensations,
and it often chooses the scariest explanation availableheart attack, passing out, losing control. People frequently report looking around
for help, Googling symptoms, or trying to escape wherever they are. Minutes later, the intensity may drop, leaving exhaustion, embarrassment,
and a deep fear of it happening again. Many describe the aftermath as a “hangover” of dread: shaky, sensitive, and on edge.
The “nighttime doom” that hits when the world is quiet
Another classic experience happens at night. Someone wakes up with a racing heart and a heavy sense that something is wrong. The room is quiet,
which means the brain has fewer distractions, so it zooms in on every internal sensation: heartbeat, breathing, stomach gurgles, random muscle
twitches. People describe lying there thinking, “Why does my chest feel weird?” or “What if I stop breathing in my sleep?”
This version often includes “checking” behaviors: checking the pulse, checking the phone time repeatedly, checking symptoms online.
Ironically, checking usually increases fear. The doom grows until the person sits up, turns on lights, drinks water, or walks around
to prove they’re okay. Over time, this can create a frustrating routine where bedtime itself becomes the triggerbecause the brain remembers
last night’s alarm.
The “my body knows something my brain can’t explain” medical scare
Some people describe impending doom as a sudden, icy certainty paired with very physical warning signs: struggling to breathe, chest pain,
swelling, hives, dizziness, or feeling faint. In these cases, the fear isn’t “random”it’s arriving alongside a body crisis.
People sometimes say, “I couldn’t explain it, but I knew I needed help,” and they seek emergency care. Clinicians often take these stories
seriously, especially when symptoms point to allergic reactions, heart problems, lung clots, or other urgent issues.
A key detail in these experiences is speed plus severity. Instead of gradually building worry, the person goes from fine to not-fine quickly.
They may feel clammy, weak, short of breath, or dizzy. The “doom” feeling can be the mind’s interpretation of a real physiological emergency
which is why red-flag symptoms should never be ignored.
The “stress bucket overflow” version
There’s also a slower-burning experience where impending doom is less like a lightning strike and more like a weather system moving in.
Someone under chronic stressschool pressure, family conflict, job insecurity, grief, or nonstop responsibilitiesmay notice a constant
background dread: “Something bad is coming.” It might spike in the mornings, before social events, or after scrolling intense news.
People often describe this as being unable to relax even when things are objectively okay. The body stays tense, the stomach is unsettled,
and sleep is lighter. In this version, the “doom” can function like an emotional smoke alarm triggered by overload rather than a single acute event.
Support, therapy, better sleep, reduced stimulant use, and practical stress changes can gradually lower the baseline so the brain stops expecting
disaster as the default setting.
If any of these experiences feel familiar, the best next step is not self-diagnosisit’s building a clearer map: what happens, when it happens,
what symptoms come with it, and what helps. That map turns an invisible fear into usable information, and usable information is the opposite of doom.