Table of Contents >> Show >> Hide
- What “Low Risk” Actually Means (and What It Doesn’t)
- What’s Going On With Bird Flu in the U.S. Right Now
- Who Is Actually at Higher Risk
- How Bird Flu Spreads to Humans
- Symptoms: What Bird Flu Can Look Like in People
- What to Do If You Were Exposed (or Think You Might Be Sick)
- Prevention That’s Boring, Effective, and Surprisingly Doable
- Why Seasonal Flu Shots Still Matter (Even Though They Don’t Prevent H5)
- Vaccines, Stockpiles, and Preparedness: Where Things Stand
- FAQ: The Questions People Actually Ask
- What This Means for Everyday Life
- Experiences From the Real World: What Bird Flu “Feels Like” in 2024–2025
“Bird flu” sounds like the kind of headline that makes you stare at your chicken nugget like it just blinked.
But the CDC’s repeated message after recent U.S. human infections has been consistent: the risk to the general public remains low.
That doesn’t mean “ignore it forever.” It means: don’t panic-buy hazmat suitsbut do pay attention to what’s happening, who’s actually at risk,
and what simple steps keep this from becoming a bigger problem.
In 2024 and 2025, the story got more complicated (and more interesting) because highly pathogenic avian influenza (HPAI)most often discussed as H5N1
showed up not only in wild birds and poultry, but also in U.S. dairy cows. That created new exposure pathways for certain workers and new questions
for public health agencies. Meanwhile, a rare subtype (H5N5) was confirmed in a Washington State patient in late 2025, underscoring the reason health officials
keep saying two things at once: low risk now, but serious monitoring.
What “Low Risk” Actually Means (and What It Doesn’t)
When the CDC says the public risk is “low,” it’s not a vibe. It’s a judgment based on real-world signals:
how often humans are getting infected, whether infections are mostly linked to direct animal exposure, andmost importantlywhether there’s evidence of
sustained person-to-person spread.
Low risk does not mean “zero risk”
People can get infected. Recent U.S. cases have included mild illnessoften featuring eye redness (conjunctivitis)as well as
occasional severe illness. But what has not been seen as an ongoing pattern in the U.S. is the kind of easy, continuous human-to-human transmission
that would change everyday life for everyone.
Low risk does mean “most people won’t encounter enough virus to get sick”
For the average person buying groceries, walking the dog, or living life normally, the odds of getting a meaningful exposure to avian influenza are very low.
The higher-risk situations are typically specific and practical: handling infected animals, cleaning contaminated environments, or having a PPE-free encounter
where virus gets into the eyes, nose, or mouth.
What’s Going On With Bird Flu in the U.S. Right Now
Avian influenza viruses circulate naturally in wild birds worldwide. The current era of H5 viruses has been unusually persistent in birds and has spilled over
into multiple animal species. In the U.S., the CDC has highlighted that H5 bird flu activity involves wild birds, poultry, and dairy cows, with sporadic human cases
linked to animal exposure.
A quick timeline you can actually follow
-
Early 2024: H5N1 is detected in U.S. dairy cattle, and a human case associated with cattle exposure is reported. Public health agencies
emphasize that the general public risk remains low. - Late 2024: The CDC confirms a severe U.S. human case of H5N1 and reiterates that this does not change the overall low public risk assessment.
-
2025: Monitoring continues for people with animal exposures, clinical guidance is updated, and public health messaging remains focused:
low risk for the general public, higher risk for certain workers and exposures. -
Late 2025: A rare subtype, H5N5, is confirmed in a Washington State patient; state and local officials again emphasize
low risk to the public while monitoring contacts.
If this feels like a lot of alphabet soup (H5N1, H5N5), you’re not alone. The key point is simpler:
the virus is widespread in animals, and human infections remain uncommonwith most linked to close contact with infected animals
or contaminated environments.
Who Is Actually at Higher Risk
“Public risk is low” is true in general, but it’s not evenly distributed. Certain jobs and activities create a bigger chance of exposureespecially when
people work close to animals, bodily fluids, or enclosed environments where virus may be present.
Groups with higher exposure risk
- Dairy and poultry workers (especially during outbreaks or when animals are sick)
- Backyard flock owners handling sick or dead birds, cleaning coops, or disposing of carcasses
- Veterinarians and animal health staff
- Hunters and wildlife rehabilitators handling wild birds or mammals
- Lab personnel working with specimens
This is why the CDC emphasizes workplace safety planning and personal protective equipment (PPE) for people who may encounter infected animals or contaminated settings.
If you’re not in these groups, the main “risk reduction strategy” is pretty boringin a good way: avoid direct contact with sick/dead animals and don’t drink raw milk.
How Bird Flu Spreads to Humans
Bird flu is primarily an animal disease. Humans are typically infected when enough virus gets into the eyes, nose, or mouth,
or is inhaled. That can happen through direct contact with infected animals, their secretions, or contaminated environments.
The “eyes matter” detail most people miss
In recent U.S. cases, conjunctivitis (pink eye) has been a prominent symptom. That’s a clue that eye exposuresplashes, aerosols, or contaminated
hands touching the facecan be an important route. It’s also why recommended PPE often includes unvented or indirectly vented goggles.
What about food?
This is where you can exhale a little. The FDA has repeatedly stated that pasteurization inactivates H5N1, and testing of pasteurized retail dairy products has not
found viable (infectious) virus. Proper cooking also reduces risk. The bigger concern is unpasteurized (raw) milk and direct exposure during animal handling,
not your grilled cheese.
Symptoms: What Bird Flu Can Look Like in People
Symptoms in humans can range from none or mild illness to severe disease. In the U.S. context, many detected cases have been mild, but severe illness has occurred.
Knowing the symptom list matters most if you’ve had recent animal exposure.
Commonly reported symptoms
- Eye redness/irritation (conjunctivitis)
- Fever or feeling feverish
- Cough, sore throat, runny or stuffy nose
- Body aches, headache, fatigue
- Sometimes GI symptoms like nausea, vomiting, or diarrhea
When to take it seriously
If you develop symptoms after contact with sick/dead birds, dairy cows, poultry operations, or a contaminated environment, treat it like a “don’t wait and see” moment.
Call a healthcare provider, describe the exposure, and ask about testing and treatment. In influenza, timing matters.
What to Do If You Were Exposed (or Think You Might Be Sick)
You don’t need to memorize a flowchart. Use a simple decision rule: exposure + symptoms = act quickly.
Public health recommendations commonly include monitoring for symptoms for a period after exposure and getting evaluated if symptoms develop.
Step-by-step, without drama
- Don’t “tough it out.” If you had a meaningful exposure and you’re symptomatic, contact a clinician and share the exposure history early.
- Ask about antivirals. CDC clinical guidance supports starting oseltamivir (Tamiflu) as soon as possible for suspected or confirmed cases.
- Follow public health guidance. In many exposure situations, people may be monitored for symptoms for a set window after the last exposure.
- Protect others while you’re figuring it out. If you’re sick, avoid close contact, practice good hygiene, and follow clinician/public health advice.
The practical goal is twofold: help the patient recover and keep an unusual virus from getting opportunities to spread or mix with other influenza viruses.
Prevention That’s Boring, Effective, and Surprisingly Doable
For the general public
- Avoid direct contact with sick or dead birds and animals.
- Keep kids and pets away from carcasses or visibly ill wildlife.
- Wash hands after being outdoors, gardening, or handling animal-related items.
- Cook poultry, eggs, and meat properly.
- Avoid raw milk and raw-milk products, especially during ongoing animal outbreaks.
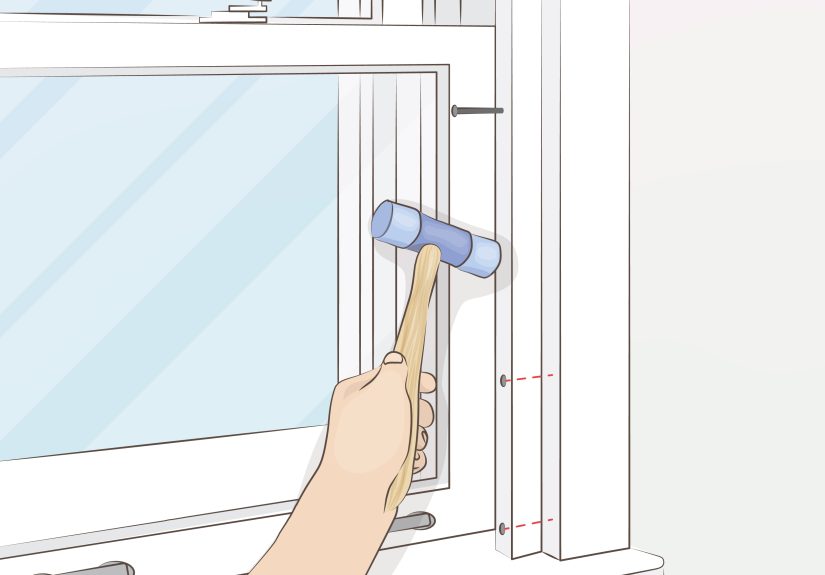
For backyard flock owners
- Limit contact between domestic birds and wild birds (feed/water placement matters).
- Use dedicated footwear or boot covers for coop areas; disinfect tools.
- Wear gloves and eye protection when cleaning or handling birds, especially if illness is suspected.
- Report unusual die-offs to local animal health authorities.
For workers in higher-risk settings
If your job involves poultry, dairy cattle, or potentially infected environments, PPE isn’t “extra.”
It’s the difference between a routine workday and a phone call that starts with, “So… about your eye redness.”
CDC interim recommendations describe PPE layers that commonly include a fit-tested respirator (like an N95), eye protection, gloves, and protective clothing.
Why Seasonal Flu Shots Still Matter (Even Though They Don’t Prevent H5)
Here’s one of public health’s least intuitive messages: the seasonal flu vaccine isn’t designed to protect against H5 bird fluyet the CDC still encourages
seasonal flu vaccination, including among people with frequent animal exposure.
The logic is practical. Reducing ordinary influenza infections reduces strain on healthcare systems and may reduce the chance of a person being infected with
two influenza viruses at once. That matters because influenza viruses can change, and public health strategy often focuses on reducing opportunities for
“bad luck + biology” to team up.
Vaccines, Stockpiles, and Preparedness: Where Things Stand
The U.S. approach to avian influenza is less “we vaccinate everybody tomorrow” and more “we prepare for if the situation changes.”
That includes surveillance, candidate vaccine development, and maintaining certain countermeasures for higher-risk scenarios.
At the moment, the headline you should remember is the same one CDC keeps repeating: without sustained person-to-person spread, the general public risk remains low.
Preparedness is about being ready before risk changes, not after.
FAQ: The Questions People Actually Ask
Should I stop eating chicken, eggs, or dairy?
No. Properly handled and cooked poultry and eggs are safe, and pasteurized dairy is considered safe by U.S. food safety authorities. The bigger avoidable risk is raw milk.
Do I need to wear a mask at the grocery store because of bird flu?
For bird flu specifically, most people do not need to change their daily routine. The risk is tied to direct animal exposure, not typical retail shopping.
What’s the “watch this closely” part?
Viruses evolve. Public health agencies watch for genetic changes, clusters of human cases, and signs of person-to-person transmission.
Monitoring exposed individuals for symptoms after animal contact is one way to catch problems earlywhile they’re still small.
What This Means for Everyday Life
The most honest summary is also the least clickbait: bird flu is a real animal outbreak with occasional human infections.
The CDC’s “low risk” label for the general public reflects current evidence, not wishful thinking. The practical response is targeted:
focus protection on higher-risk exposures (workplaces, farms, backyard flocks), keep food safety habits strong, and improve detection and treatment pathways.
If you’re not directly handling birds or livestock, your part is simple: don’t touch sick or dead animals, avoid raw milk, and stay informed from reliable sources.
That’s not a thrilling hero narrativebut it’s exactly how public health wins.
Experiences From the Real World: What Bird Flu “Feels Like” in 2024–2025
Statistics are great for scientists and spreadsheets, but most people want to know what this looks like in real life. The lived experience of “bird flu risk”
in the U.S. has been less like a blockbuster movie and more like a series of very specific, very human momentsmost of them happening far away from the average
person’s day-to-day routine.
For some dairy and poultry workers, the experience starts with a strangely ordinary problem: an animal is “off.” A dairy worker might notice cows eating less,
producing less milk, or producing milk that looks abnormal. On a poultry farm, it can move faster and more dramaticallybirds can become sick quickly and die in clusters.
The emotional tone isn’t panic; it’s urgency mixed with practicality. People still have a job to do, animals still need care, and every new protocol adds time and friction.
PPE can feel hot, annoying, and slow. But workers who have lived through outbreaks often describe a shift: once you’ve seen how fast respiratory viruses can derail a workplace,
wearing goggles and a respirator feels less like overkill and more like not wanting to spend your weekend at urgent care explaining why your eye looks like a tomato.
Clinicians and public health staff experience a different kind of “busy.” When someone with a relevant exposure shows up with pink eye and mild flu symptoms,
it creates a small, focused scramble: collecting the right specimens, ensuring the lab knows this is a novel influenza concern, and deciding whether to start antivirals promptly.
Many providers describe these investigations as “high attention, low volume.” In other words, they aren’t seeing bird flu patients all day longbut when a suspected case appears,
the case demands careful steps, fast communication, and follow-up. Contact monitoring can also feel odd for families: people who had close contact with the patient may be asked
to monitor for symptoms for days, take their temperature, or check in with health officials. Most of them never develop illness, which is reassuringbut the process itself can be
stressful because it turns normal life into a countdown.
Backyard flock owners often describe the experience as heartbreak plus homework. Many people keep chickens as pets, not as “poultry production.”
When wild birds migrate through or when a neighbor mentions a die-off, flock owners start Googling biosecurity tips and realizing their coop setup was designed for cuteness,
not containment. They may add barriers to keep wild birds out of feed and water, disinfect more carefully, or reduce visitors to the coop area.
Some owners talk about the guilt of “Did I do something wrong?” even when the answer is nowildlife exposure is hard to control completely.
And when a human case makes headlines, the fear can jump the fence: people wonder if their children are at risk from collecting eggs or helping with chores.
The real-world reassurance is that risk is still low for the general public, but it feels more personal when it’s your own yard.
Finally, the public’s experience is often shaped by information overload. One day the headline is “risk is low,” the next day it’s “new strain,” and the human brain does
what it always does: it tries to turn uncertainty into certainty. Some people respond by dismissing the story entirely; others respond by assuming the worst.
The healthiest middle grounddescribed by many who work in public healthis to treat bird flu like a monitored hazard: stay calm, take smart precautions if you’re in a higher-risk group,
and support the boring systems that keep risk low (testing, surveillance, PPE, food safety).
In a way, the most common American experience of bird flu is this: life continues normally precisely because the response is targeted and persistent, even when it’s not dramatic.