Table of Contents >> Show >> Hide
- 1) Faster, safer decisions with connected records, smart ordering, and barcode checks
- 2) Less uncertainty with real-time updates and clearer communication
- 3) A more human visit through virtual care, remote monitoring, and accessibility tech
- Bringing it together: technology that feels like care, not clutter
- Experiences from the ER: what these technologies feel like as a patient (and family)
- SEO tags (JSON)
The emergency room is a weird place: it’s part life-saving pit crew, part air-traffic control tower, and part “why is the vending machine out of pretzels again?”
If you’ve ever been in an ER, you know the vibe can swing from calm to chaos in the time it takes a blood pressure cuff to inflate.
The good news: a lot of today’s emergency department (ED) technology isn’t about adding more screens for staff to stare at (though… yes, there are screens).
The best tech is the kind that quietly makes your visit safer, clearer, and less stressfulwithout you needing an IT degree or a secret password.
Let’s break down the three biggest ways technology in the ER boosts the patient experiencewhat it is, how it works, and what it feels like from the patient side.
1) Faster, safer decisions with connected records, smart ordering, and barcode checks
In an emergency, time mattersbut so does accuracy. The ER doesn’t just need “fast.”
It needs “fast, correct, and consistent,” which is basically the holy trinity of not making a bad day worse.
Instant access to your story (even when you can’t tell it)
Electronic health records (EHRs) and health information exchange help clinicians see critical details quickly: medications, allergies, problem lists,
prior visits, recent labs, imaging, and discharge notes. When this information is available at the point of care, it can reduce delays,
prevent repeat tests, and help teams make better decisionsespecially when patients are in pain, confused, or unable to speak for themselves.
Sources:
Example: A patient comes in with shortness of breath and a history of heart failure. If the ER team can quickly confirm prior echocardiogram results,
recent medication changes, and previous hospitalizations, they can tailor treatment sooner. That can mean fewer “let’s re-do everything” steps,
and more “let’s do the right thing first” steps.
Another big patient-experience win: care coordination. When the ED can share or retrieve information across settings (primary care, specialists,
pharmacies, other hospitals), handoffs tend to be smootherand patients spend less time repeating their life story like a podcast with no skip button.
Sources:
Clinical decision support: the quiet double-checker
Many EHR systems include clinical decision supportalerts and prompts that help reduce common errors and improve safety.
Think: drug-allergy warnings, medication interaction flags, reminders for evidence-based protocols, and order sets that standardize care during high-pressure moments.
Done well, this is like having a calm second set of eyes in a loud room.
Sources:
That matters for patient experience because safety is experience. Patients might not see the alert pop up, but they feel the result:
fewer mix-ups, more consistent care, and less “wait, what medication did you say you take again?”
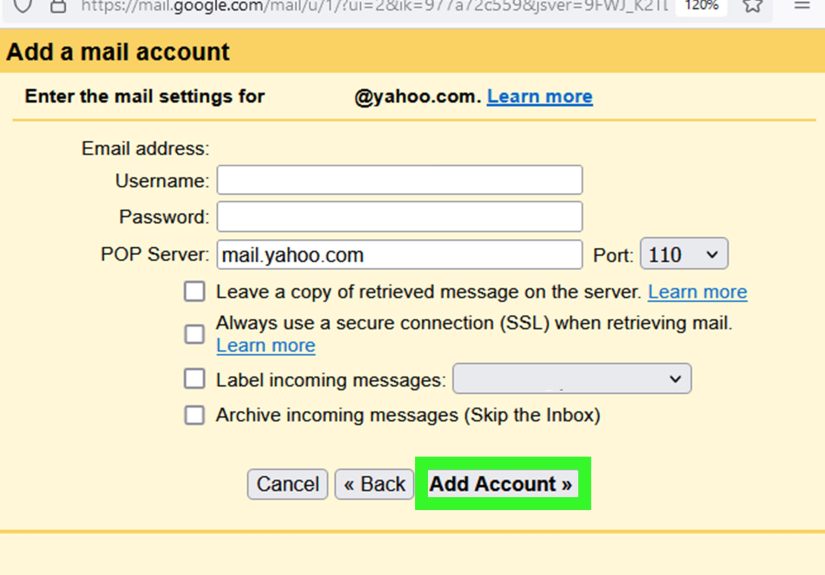
Barcodes and wristbands: fewer “Oops” moments
Barcode medication administration (BCMA) is one of the most practical safety technologies in hospitals.
The basic idea: scan the patient’s wristband and the medication to confirm the right patient, right drug, right dose, right time, and right route.
Studies and patient-safety reviews have found that barcode-based processes can reduce medication administration errors.
Sources:
This pairs nicely with patient identification best practiceslike using at least two identifiers (for example, name and date of birth) before giving medications,
drawing labs, or doing procedures. It may feel repetitive when staff ask you the same questions again and again, but it’s a feature, not a bug.
Sources:
Patient experience translation: fewer errors, fewer delays caused by re-checking, and more confidence that the care team is getting it right.
(Also, that little barcode scanner “beep” is basically the sound of your safety net tighteningcomforting, in a slightly robotic way.)
2) Less uncertainty with real-time updates and clearer communication
Ask people what they dislike most about an ER visit, and you’ll hear some variation of:
“I didn’t know what was happening,” “I didn’t know how long it would take,” and “I didn’t know who to ask.”
Technology can’t erase every delaybut it can reduce the stress that comes from uncertainty.
Tracking tools and smarter flow: fewer lost minutes (and fewer lost humans)
EDs use patient-tracking tools to improve “patient flow”the movement from arrival to triage to testing to treatment to discharge or admission.
Some hospitals use real-time location systems (RTLS) or similar tracking approaches to help staff locate patients, equipment, and care teams,
which can reduce bottlenecks and improve coordination.
Sources:
Even when patients never see the behind-the-scenes dashboards, they feel the improvements:
- Less time waiting for someone to find equipment or an open room
- Fewer “we’re still trying to track down…” delays
- More predictable steps (triage → labs → imaging → results → plan)
A smoother process doesn’t just help the hospital run betterit makes the patient experience feel more organized and less random.
In the ER, “organized” is a love language.
Wait-time transparency: the magic is being kept informed
Some EDs communicate updates through digital signage, estimated wait-time displays, or text-message systems that let patients receive updates
and sometimes wait in a less crowded area. Research on SMS-based updates in ED settings has explored improving satisfaction with wait time,
largely by changing the experience of waitingbecause informed waiting is less frustrating than silent waiting.
Sources:
This isn’t about pretending the wait is shorter. It’s about reducing the emotional tax of “What’s going on?”
A simple message like “Lab results are pending; next step is provider evaluation” can be surprisingly calming.
And it helps families too. When loved ones aren’t guessing, they’re less likely to panic, hover, or spiral into worst-case scenarios
based solely on the fact that it’s been 45 minutes and no one has appeared.
Clearer bedside communication: digital tools, whiteboards, and shared plans
“Communication boards” (sometimes literal whiteboards, sometimes digital equivalents) are used to keep patients updated on care team members,
plan-of-care details, and next steps. Patient-safety and patient-experience resources note that tools like this can support patient-centered communication
and reduce confusionespecially in busy hospital environments.
Sources:
In ER terms, the best communication is:
- Specific: “We’re waiting on your CT scan results” beats “We’ll see.”
- Honest: “It may take another hour” beats “Soon.”
- Actionable: “If your pain changes, hit the call button” beats “Try to relax.”
Technology helps create a single, consistent story so you don’t get three different answers from three different people,
whichlet’s be realcan make patients feel like they’re in the plot of a medical mystery show they didn’t sign up to binge.
3) A more human visit through virtual care, remote monitoring, and accessibility tech
Here’s the twist: some of the best ER technology doesn’t make care feel more “high-tech.”
It makes care feel more human by reducing friction, improving access, and helping patients understand what’s happening.
Virtual triage and “provider in triage”: faster evaluation and better prioritization
A growing approach in emergency medicine is using telehealth or virtual provider models to improve throughputlike virtual provider triage
or technology-supported “fast track” workflows. Research in emergency medicine has described how virtual triage programs can improve efficiency
and affect outcomes like “left without being seen,” which matters because leaving before evaluation is a bad outcome for both safety and experience.
Sources:
What this looks like in real life:
- A clinician evaluates you sooner (sometimes via video) to start orders earlylabs, imaging, pain control, or EKGs.
- You may get moved to the right pathway faster (urgent care referral, discharge with follow-up, or full ED workup).
- The ED can reserve rooms for patients who truly need them, which can reduce crowding and delays.
Patient experience translation: less limbo, more progress. Even if the total visit is still long, the first meaningful step happens sooner.
And psychologically, that’s huge.
Remote monitoring and smarter alerts: safer care without constant interruptions
Modern monitoring includes wireless or centralized systems that help teams detect changes soonerlike oxygen saturation drops, heart rate changes,
or abnormal vital sign trends. Not every ED uses the same tools, but the general trend is clear: better monitoring supports earlier intervention,
which improves safety and can reduce the “wait until it gets worse” risk.
It can also reduce unnecessary interruptions. When staff have clearer data and smarter alerts, they may not need to “pop in” as frequently just to re-check
something that a connected monitor is already tracking. That means fewer disruptions for resting patients and fewer anxious “is something wrong?” moments
when someone rushes into the room unexpectedly.
Accessibility and understanding: language support, discharge clarity, and portals
A good ER visit isn’t just about what happens in the departmentit’s about what you understand when you leave.
Patient-facing digital tools (including patient portals and electronic after-visit summaries) can support engagement by making instructions,
results, and follow-up plans easier to access and revisit. Research on patient portals has found associations with patient engagement and perceived usefulness,
though adoption and usability vary widely.
Sources:
Add language access tools (like video interpretation or on-demand interpreter services), and the patient experience improves in a very basic, powerful way:
patients can understand what’s happening, ask questions, and make informed decisions.
When patients feel heard and informed, the ER becomes less intimidating. Tech can’t replace empathybut it can make empathy easier to deliver at scale,
especially on the busiest nights when everyone is running on adrenaline and cafeteria coffee.
Bringing it together: technology that feels like care, not clutter
The best ER technologies share a goal: reduce risk, reduce confusion, and reduce friction.
When records are connected, teams can treat faster and safer. When updates are clearer, waiting feels less stressful.
When virtual care and accessibility tools are used well, patients feel more supported and less lost.
Of course, technology isn’t magic. Bad implementations can frustrate staff and patients alike.
But when the tools are designed around real workflowsand when clinicians can keep their focus on people, not pop-upstechnology in the ER can
genuinely boost the patient experience.
Sources:
In other words: the goal isn’t an ER that feels like a spaceship. It’s an ER that feels like a place where the right things happen reliably,
and you’re never left wondering what happens next.
Experiences from the ER: what these technologies feel like as a patient (and family)
To make this more real, here are common experience patterns patients and families describebased on how modern ED workflows tend to play out when technology is
used thoughtfully. These are illustrative composites (not individual stories), but they reflect the kinds of moments that shape whether an ER visit feels chaotic
or cared-for.
The “I’m still waiting, but I’m not panicking” text update
One of the strangest parts of the ER is that waiting can feel like nothing is happeningeven when a lot is happening behind the scenes.
Patients often say the hardest part isn’t the time itself; it’s the uncertainty. A text update, a status screen, or a quick digital note that says,
“Your bloodwork is in process; imaging is next,” can turn the wait from a blank void into a timeline with steps.
Families notice this too. Instead of imagining worst-case scenarios, they can anchor their expectations:
“Okay, labs first. Then the doctor. Then we’ll know.” It’s not that anyone loves waiting. It’s that being kept informed feels respectful.
The “beep” that builds trust
Patients don’t always know what BCMA isand frankly, nobody should need a glossary while wearing a paper gown.
But people do notice when a nurse scans a wristband and scans a medication. That small ritual can feel like, “They’re checking. They’re careful.”
In a place where you’re vulnerable and possibly scared, visible safety steps build confidence.
There’s also a subtle emotional benefit: patients feel less like a “room number” and more like a person whose identity matters.
(And yes, the nurse may still ask your name and birthday right after scanningbecause redundancy is how safety systems stay safe.)
The early evaluation that changes the whole tone of the visit
Many patients describe a turning point in the visit: the moment it feels like care is actually underway.
When virtual triage or “provider in triage” models work well, that turning point happens earlier. Even a brief initial evaluation can help:
pain relief started sooner, labs ordered quickly, an EKG performed without delay, or reassurance that symptoms don’t signal something immediately life-threatening.
The total visit may still take hoursbecause medicine takes time. But patients often say, “At least things started moving.”
That forward motion matters for comfort and confidence.
The discharge instructions you can actually follow
The end of the ER visit can be a blur: relief, exhaustion, maybe embarrassment about how dramatic your symptoms felt at 2 a.m. (Don’t worryER staff have seen it all.)
Digital discharge instructions, patient portals, and electronic summaries can help patients revisit what they were told when their brain is finally back online.
Patients often appreciate being able to check medication changes, follow-up steps, and warning signs laterespecially if they were groggy, in pain,
or juggling a worried child or older parent. When information is easier to access, patients are more likely to do the right next step:
follow up with primary care, fill the prescription correctly, or return if symptoms worsen.
The most human moment: understanding
Technology is at its best when it helps patients understand. Whether that’s interpreter access, clearer written plans, or consistent updates,
the emotional “win” is the same: patients feel less alone in a stressful environment. They feel oriented.
And in the ER, feeling oriented is a form of comfortalmost as valuable as a warm blanket that’s actually warm.