Table of Contents >> Show >> Hide
- What “Public Health Emergency” Actually Means (and What It Doesn’t)
- Why End the PHE in May?
- What Changed After May 11, 2023
- 1) COVID-19 tests: “free” became “it depends”
- 2) Vaccines: still available, but the payment system shifted
- 3) Treatments: more normal healthcare rules, less emergency scaffolding
- 4) Telehealth: some flexibilities continued, but not all
- 5) Medicaid coverage: the “unwinding” was bigger than one date
- 6) Hospitals and providers: waivers sunset, operations recalibrate
- What Stayed the Same (Because Viruses Don’t Read Press Releases)
- How to Navigate the Post-PHE World Without Losing Your Mind
- The Big Picture: Ending Emergency Mode Without Ending Preparedness
- What the Transition Felt Like: Real-World Experiences (May 2023 and After)
- Conclusion
When the U.S. government says it’s ending a “public health emergency,” it can sound like someone’s about to flip a giant switch labeled
Pandemic: OFF. In reality, it’s more like retiring an old backstage pass: the show is still happening, but the crew can’t use the same shortcuts.
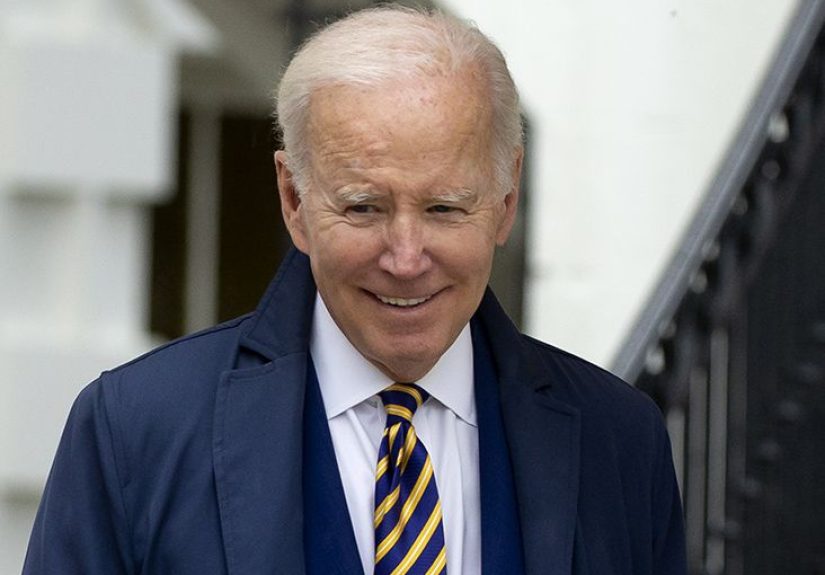
In early 2023, the Biden administration confirmed it would let the federal COVID-19 Public Health Emergency (PHE) expire in Mayspecifically on
May 11, 2023. That date mattered because thousands of policies, payments, and temporary healthcare flexibilities were tied (directly or indirectly)
to the PHE timeline. Some ended immediately, some tapered off, and some had already been extended by Congress long before the May deadline.
This article breaks down what the PHE was, why ending it wasn’t the same as “declaring victory,” and what changed for regular peopleespecially around
vaccines, testing, telehealth, Medicaid coverage, and the healthcare system’s “emergency mode” paperwork.
What “Public Health Emergency” Actually Means (and What It Doesn’t)
The COVID-19 Public Health Emergency was a legal status declared by the Secretary of Health and Human Services under federal law. Think of it as an
official permission slip that let federal agencies move faster, waive certain requirements, and fund pandemic-era programs more flexibly.
Emergency declarations aren’t all the same thing
One reason the public got whiplash is that “the emergency” was really a stack of different emergency authorities. The big ones were:
- The HHS Public Health Emergency (PHE): triggered healthcare flexibilities and certain coverage rules.
- The presidential “national emergency”: a separate declaration under the National Emergencies Act.
- Other authorities: separate policies and laws that could continue regardless of the PHE’s status.
In fact, Congress moved on the national emergency earlier than the original May plan. A joint resolution signed in April 2023 terminated the COVID-19
national emergencywhile the PHE still ran to May 11. That’s not a contradiction; it’s bureaucracy doing what bureaucracy does best: filing things in
different folders.
Ending the PHE didn’t impose new restrictions
Another misconception: that keeping the PHE active meant masks or vaccine mandates were automatically in place. The administration’s own policy statement
emphasized that continuing the emergency declarations did not, by itself, force day-to-day behavior changes like mask mandates or school closures.
By 2023, most public restrictions had already been lifted or shifted to local decision-making.
Why End the PHE in May?
By early 2023, the U.S. response to COVID-19 had changed dramatically from the frantic early days of 2020. Vaccines and treatments were widely available,
hospitals weren’t operating under constant surge conditions in the same way, and policymakers were trying to migrate COVID management into “normal”
public health operations.
There was also a practical reason: the healthcare system needed runway. The administration argued that ending emergency authorities abruptly could create
chaos for patients, states, hospitals, and insurersso it aligned the expiration with prior commitments to give advance notice before terminating the PHE.
In other words: less surprise, fewer frantic memos, fewer people discovering “the rules changed yesterday” when they’re already stressed.
Politics played a role too. Congress was debating proposals to end emergency declarations earlier. The administration’s approach was essentially:
“We’re ending itbut we’re doing it with a calendar and a plan, not by yanking the cord mid-sentence.”
What Changed After May 11, 2023
1) COVID-19 tests: “free” became “it depends”
During much of the pandemic, many people got used to a magical era when COVID tests showed up in the mail like very unglamorous gifts.
As the PHE ended, the guarantee of no-cost coverage for certain testing scenarios weakened. Private insurers and public programs could still cover tests,
but they were no longer operating under the same blanket requirements that existed during emergency response mode.
Practical takeaway: after May 2023, many people started encountering more variationsome plans covered over-the-counter tests, others didn’t,
and “free testing” became more likely to depend on a provider order, a specific benefit design, or local programs.
2) Vaccines: still available, but the payment system shifted
Vaccines didn’t disappear when the PHE ended. But the financing and distribution model shifted over time as the federal government transitioned away
from directly purchasing and supplying doses in the same way it had during the height of the emergency response.
For many insured people, coverage continued through health plans, with policy details depending on plan type and updated recommendations.
For uninsured and underinsured adults, federal and state partners later rolled out programs to preserve access at participating sites, including pharmacies
and health departmentsaimed at reducing the “I want a shot but I can’t afford it” problem.
3) Treatments: more normal healthcare rules, less emergency scaffolding
Antiviral treatments and therapeutics remained important tools, particularly for higher-risk people. But, as with tests and vaccines, the post-PHE world
leaned more heavily on the standard healthcare payment ecosystem: insurance coverage rules, provider networks, and clinical pathways that look more like
“regular medicine” and less like “emergency deployment.”
4) Telehealth: some flexibilities continued, but not all
Telehealth is the pandemic policy that refused to quietly pack up and leaveand millions of patients were glad about that.
Many Medicare telehealth flexibilities were extended by legislation beyond the PHE timeframe. That meant May 11 did not automatically equal
“telehealth over.” It was more like “telehealth enters its long-term relationship phase,” complete with negotiations, fine print, and awkward questions like:
“So… what are we now?”
Still, the PHE ending mattered because some waivers and temporary policies were explicitly tied to emergency authority. Providers had to track which
telehealth services were extended by law, which depended on payer policies, and which were returning to pre-pandemic rules. Patients experienced this as:
some virtual visits stayed easy, while others required new steps or reverted to in-person requirements depending on location, provider type, and coverage.
5) Medicaid coverage: the “unwinding” was bigger than one date
If you want to understand why the PHE ending was a big deal, zoom in on Medicaid.
During the pandemic, states received enhanced federal funding in exchange for keeping many people continuously enrolledmeaning fewer coverage losses
during a public health crisis.
By 2023, the country moved into a massive “unwinding” period: states restarted eligibility reviews and renewals at scale. That process was not just
a paperwork exercise; it affected real people who had moved, changed jobs, aged into a different eligibility category, or simply missed a letter.
Many policy bulletins and guidance documents emphasized practical stepslike updating contact information, responding to renewal notices, and seeking help
if coverage was terminated incorrectly. The big headline was simple: the safety net was still there, but you might need to re-prove you qualify to keep it.
6) Hospitals and providers: waivers sunset, operations recalibrate
The PHE enabled a buffet of waivers and flexibilities for healthcare providersuseful in a crisis, messy to maintain forever.
As the emergency ended, healthcare organizations had to transition back toward standard conditions of participation, reporting requirements,
and operational rules.
Some changes were immediate; others had transition periods. For patients, this often showed up indirectlythink different discharge practices,
changes in how certain services were billed, or fewer “pandemic exceptions” in how care could be delivered.
For administrators, it showed up as a small avalanche of compliance checklists (the least fun kind of confetti).
What Stayed the Same (Because Viruses Don’t Read Press Releases)
Ending the PHE didn’t mean COVID-19 stopped circulating or stopped harming peopleespecially older adults and those with underlying health conditions.
Public health agencies continued tracking trends, updating guidance, and encouraging vaccination and treatment for those at risk.
Many core tools remained available: updated vaccines, diagnostic testing, and therapeutics. The shift was less about “do we care?” and more about
“how do we pay for this, regulate it, and manage it sustainably?”
Another subtle but important change: certain types of data collection and reporting authorities tied to the PHE ended, requiring agencies to adapt how they
monitor the virus and communicate risk. Over time, COVID reporting became more like reporting for other respiratory diseasesless constant, more targeted,
and (sometimes) less granular than the public had grown used to.
How to Navigate the Post-PHE World Without Losing Your Mind
“Post-PHE” doesn’t have to be scary. It mostly means you should expect more variationbetween insurance plans, between states, and between providers.
Here’s how people generally avoided unpleasant surprises:
Check your coverage rules before you need care
- Look up whether your plan covers at-home tests and under what conditions.
- Confirm where you can get vaccinated with the lowest out-of-pocket cost.
- Ask your provider’s office whether telehealth is covered for your visit type.
If you or your family uses Medicaid, treat mail like it’s important again
During the unwinding, a surprisingly common problem wasn’t “ineligible,” it was “never got the notice.”
If your address, phone number, or email changed, updating it became a health insurance survival skill.
Know that “free” may now come from local programs, not universal rules
Community health centers, local health departments, and pharmacy programs continued to play a big role in accessespecially for uninsured or underinsured
populations. The difference after the emergency: access was often delivered through programs and partnerships instead of broad emergency mandates.
The Big Picture: Ending Emergency Mode Without Ending Preparedness
The May 2023 decision marked a pivot: COVID-19 was moving from emergency response to long-term management. That pivot is emotionally complicated.
People wanted closure. Governments wanted sustainable policy. Healthcare systems wanted fewer temporary rules and more predictable planning.
But “sustainable” doesn’t mean “complacent.” The same years that ended the PHE also taught the country a lasting lesson: preparedness is cheaper than panic.
The goal after May 2023 wasn’t to forget COVID-19it was to build a system where responding to it doesn’t require emergency duct tape every time.
What the Transition Felt Like: Real-World Experiences (May 2023 and After)
Policy changes are usually described in spreadsheets, but people experienced the end of the PHE in everyday momentsat the pharmacy counter, in a school
nurse’s office, or while refreshing a health plan portal that always seems to log you out right when you find the right page.
For some families, the change felt subtle. A parent who used to keep a drawer full of mailed test kits noticed that replacements weren’t as automatic.
The household routine shifted: instead of “we’ll test before Grandma visits,” it became “let’s see what the store hasand what our plan reimburses.”
Nobody held a ceremony for the new routine, but it arrived anyway.
College students and young workers described a different kind of adjustment: telehealth went from “the default” to “the question.”
Many people still had virtual options, but they learned to ask in advance, “Is this appointment eligible for video?” Some clinics kept virtual follow-ups
because they worked. Others quietly nudged patients back in-person, especially for visits where a physical exam mattered.
The experience felt less like losing telehealth and more like discovering telehealth has ruleslike any relationship, it got serious.
Medicaid enrollees often felt the transition most sharply. People who hadn’t had to re-certify eligibility during the pandemic suddenly had to confirm
their information again. Community organizations reported helping neighbors navigate notices, deadlines, and document requests.
Some people were still eligible but lost coverage temporarily because a form went to an old address or the renewal packet was confusing.
The emotional tone wasn’t “the emergency ended,” it was “why is my coverage on pause when nothing about my life changed?”
Healthcare workers experienced the shift as both relief and extra work (yes, both). On one hand, emergency-era staffing and operational strain had eased.
On the other, the end of waivers meant updating policies, retraining staff, and double-checking compliance rules that had been relaxed for years.
A nurse might not think about federal declarations during a shift, but the scheduling team sure didbecause billing rules and visit types can change what
patients pay and what clinics can offer.
Pharmacists and public health staff described a “handoff” feeling: COVID tools still mattered, but the financing and logistics were changing.
Instead of federal emergency pipelines, distribution increasingly flowed through the normal channels of insurance and public programs.
People continued getting vaccinatedespecially those at higher riskbut conversations about cost and coverage became more common.
The vibe was less “crisis response” and more “ongoing maintenance,” like swapping a fire hose for a garden hose: still water, different pressure.
And for many Americans, the most honest summary was: nothing suddenly ended, but everything slowly got more complicated.
The PHE era made access feel standardized; the post-PHE era made access feel individualized. That’s not always badsome emergency rules were never meant
to last. But it did mean people had to get a little more proactive, a little more curious, and occasionally a little more stubborn on the phone with
customer service.






