Table of Contents >> Show >> Hide
If breasts could talk, they’d probably say, “We’re doing a lot more than just filling out your T-shirt.” And honestly, they wouldn’t be wrong. The human breast is a complex, multi-layered structure with jobs ranging from nourishing infants to serving as a key indicator of health changesespecially when it comes to detecting breast cancer early.
In this in-depth, easy-to-read (and sometimes fun) guide, we break down how breasts work, what’s going on beneath the skin, and how to confidently perform self-exams that could save your life. Whether you’re refreshing your knowledge or learning it all for the first time, consider this your go-to resource for understanding breast anatomy, breast function, and practical steps for breast cancer detection.
Understanding Breast Anatomy
The breast is more than meets the eyeliterally. Beneath the skin lies a carefully organized system of glands, ducts, fat, and connective tissue. Together, they form a functional network that changes throughout life depending on hormonal shifts, age, pregnancy, breastfeeding, and overall health.
Main Structures of the Breast
1. Lobules
Lobules are small, grape-like clusters responsible for producing milk. Adults typically have 15–20 lobes, each containing many smaller lobules. The number of active lobules varies depending on hormonal influences, pregnancy, and breastfeeding. While small in size, they are big players in breast functionand sometimes the origin site of certain cancers.
2. Milk Ducts
If lobules are the “factories,” ducts are the highways. These small channels carry milk from the lobules to the nipple. Most breast cancers begin in the ducts, which is why understanding duct anatomy is helpful when learning about early detection.
3. Fat Tissue (Adipose Tissue)
Fat gives breasts their shape, size, and softness. Contrary to popular belief, breast size has little to do with milk production capabilityit’s mostly just variations in the amount of fat. This tissue also helps protect internal structures and influences how breasts look and feel.
4. Cooper’s Ligaments
These fibrous, web-like bands act like internal “support straps,” helping maintain breast shape. Over time, gravity, aging, and pregnancy may stretch these ligaments, contributing to natural sagging. (Pro tip: bras do not prevent Cooper’s ligament stretching, but they do help you feel supported!)
5. The Nipple and Areola
The nipple is the central exit point for milk, while the areola contains tiny oil-producing glands called Montgomery glands, which protect the nipple during breastfeeding. The size and color of the areola vary widely and may change with hormonal fluctuations.
6. Lymph Nodes
Lymph nodes near the breastspecifically the axillary (underarm) and supraclavicular (above the collarbone) nodesplay a major role in immune defense. These nodes can become involved when breast cancer spreads, which is why doctors examine them during clinical breast exams.
What Are the Main Functions of the Breast?
Breasts have one primary biological mission: producing and delivering milk. Beyond that, they serve additional physiological and psychological functions.
1. Milk Production (Lactation)
During pregnancy, hormones like prolactin stimulate milk production in the lobules. After childbirth, an intricate hormonal danceparticularly involving oxytocinhelps push milk through ducts to the nipple. This biological design is incredibly efficient and adjusts based on the baby’s needs.
2. Immune Protection
Breast milk contains antibodies, immune cells, and nutrients that help protect infants from infection. The breast responds to a baby’s saliva during nursing, adjusting the milk’s immune profile based on the baby’s needs. Yes, breasts are basically smart home devices for infant immunity.
3. Hormone Response and Life Stages
Breasts undergo changes during puberty, menstrual cycles, pregnancy, breastfeeding, and menopause. Hormones like estrogen and progesterone influence tenderness, swelling, and density. Understanding your personal breast “baseline” helps you spot unusual changes.
4. Sensory and Emotional Roles
Breasts are rich in nerve endings and are connected to emotional bonding during nursing and intimate touch. While not often talked about, the sensory functions of breasts play a meaningful role in overall well-being.
How to Check for Breast Cancer
Early detection saves livesperiod. When caught early, breast cancer has significantly higher treatment success rates. Self-exams, mammograms, and clinical screenings all work together to help you stay informed about your breast health.
1. Know Your “Normal”
The most effective breast self-awareness technique is learning what your breasts typically look and feel like. No one knows your body better than you. If you understand your normal texture, sensitivity, and shape, you’re more likely to recognize changes early.
2. Monthly Breast Self-Exams
When to Perform It
For people who menstruate, the best time is a few days after your period ends, when breasts are least tender. For those who do not have periods, choose one consistent day monthly.
How to Perform a Self-Exam
Step 1: Visual Check
- Stand in front of a mirror with your shoulders straight.
- Look for changes in size, shape, or symmetry.
- Check for skin dimpling, redness, swelling, or changes to the nipple.
Step 2: Use Your Hands
Raise your arms, then repeat the visual exam. Follow with a hands-on exam using a circular motion with the pads of your fingers.
Step 3: Lying Down Exam
Lie down and use your right hand to check the left breast and vice versa. Make sure to cover:
- The entire breast
- The underarm area
- The collarbone region
Step 4: Shower Exam
Many people find it easiest to feel for changes with wet, soapy hands. Use gentle pressure and circular motions.
3. Warning Signs to Watch For
- Lumps, thickening, or hard knots
- Unexplained pain in the breast or nipple
- Changes in nipple direction, especially inversion
- Liquid discharge not related to breastfeeding
- Rashes or texture changes (like “peau d’orange,” or orange peel texture)
- Swelling in the breast, collarbone, or armpit
If you notice any of these signs, contact a healthcare professional promptly. Not all changes mean cancer, but all deserve attention.
4. Clinical Breast Exams
Healthcare providers often perform exams during routine checkups. These clinical exams can detect lumps or irregularities you might miss. They are recommended annually for many adults, depending on age and risk factors.
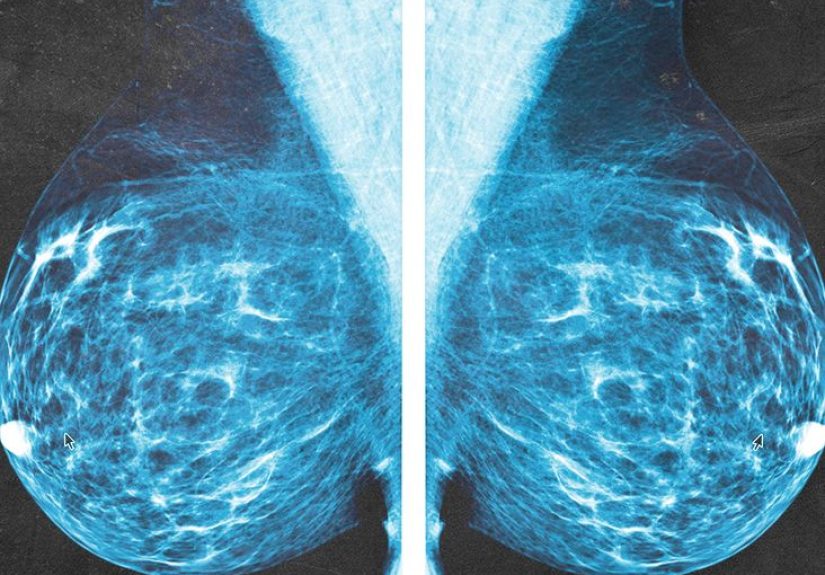
5. Mammograms
Mammograms are the most effective screening tool for early breast cancer detection. These low-dose X-rays can detect abnormalities long before they cause symptoms.
General Guidelines
- Ages 40+: Annual or biennial mammograms (varies by medical guideline)
- High-risk individuals: May start as early as age 30
- Discuss your personal risk with a healthcare provider
6. Additional Imaging
In some cases, doctors recommend ultrasound or MRI scans, especially for individuals with dense breast tissue or elevated cancer risk.
How Lifestyle and Genetics Affect Breast Cancer Risk
While you can’t control all risk factors, many lifestyle habits influence breast health. Maintaining a balanced diet, exercising regularly, limiting alcohol intake, and avoiding smoking all contribute to reduced cancer risk. Meanwhile, geneticsspecifically BRCA1 and BRCA2 mutationsplay a significant role. Knowing your family history can help you make proactive health decisions.
of Reader Experience & Insights
Breast health isn’t just medicalit’s deeply personal. For many people, the journey toward understanding breast anatomy and cancer screening starts with curiosity or a sudden scare, such as finding a lump or hearing about a friend’s diagnosis. But the more you learn, the more empowered you become.
Many individuals describe their first breast self-exam as awkward or uncertain. “Am I doing this right?” “What exactly am I feeling for?” These are normal thoughts. Over time, though, self-exams become easier, faster, and more intuitive. One common experience is discovering small lumps that turn out to be harmless cysts or fibrocystic tissuecommon conditions that can cause the breasts to feel lumpy or tender, especially before a period.
Others share stories of catching small abnormalities early thanks to routine mammograms. In many cases, cancers detected at stage 0 or stage 1 are highly treatable, with excellent outcomes. These testimonials highlight the importance of consistent screenings, even when you feel healthy.
Some people also note how breast density influences their screening journey. Dense breasts can make it harder to detect tumors on mammograms, leading doctors to recommend ultrasound or MRI imaging for better clarity. Learning whether you have dense breast tissue is a valuable part of your personal health profile.
Emotionally, breast health can stir powerful feelingsfear, vulnerability, strength, and relief. Many describe the anxiety of waiting for mammogram results, followed by immense peace when the results come back clear. Others talk about the power of community: support groups, online forums, or simply conversations with loved ones who’ve navigated similar experiences.
For those who have undergone treatmentsurgery, radiation, chemotherapy, or hormone therapytheir reflections often focus on resilience. They describe the courage it took to endure each step and the determination to prioritize their health no matter what.
If there’s a universal lesson from these experiences, it’s this: breast awareness isn’t just a routineit’s an act of self-care. Regular check-ins with your body, informed by knowledge and confidence, give you more control over your health. That’s the true heart of breast care.
Conclusion
Breasts are remarkable, complex, and constantly changing. By understanding their anatomy, appreciating their functions, and practicing regular self-checks, you strengthen your ability to detect early signs of breast cancer. Whether using self-exams, clinical screenings, or mammograms, staying proactive is the key to lifelong breast health.