Table of Contents >> Show >> Hide
- How doctors classify breast cancer: The big picture
- Carcinoma in situ: “Stage 0” breast cancer
- Invasive breast cancers: When cells break out
- Molecular and receptor types: HR+, HER2+, and triple-negative
- Common symptoms across breast cancer types
- How treatments are chosen
- Metastatic and recurrent breast cancer
- Real-life experiences: Navigating breast cancer types in the real world
Hearing the words “you have breast cancer” is terrifying. But right after that sentence,
doctors usually say a second one that matters just as much: “Here’s the type of breast cancer you have.”
That “type” isn’t just a label it strongly influences your treatment plan, your side effects, and your long-term outlook.
The tricky part? Breast cancer isn’t one single disease. It’s a big family of related but different conditions,
grouping together things like where the cancer started, whether it has spread, what fuels it, and how it behaves
under the microscope. Understanding the basics can help you feel more in control, ask sharper questions, and
better follow conversations with your care team.
This guide walks through the most common breast cancer types, their key
definitions, typical symptoms, and standard treatment options plus
some real-world insights at the end about living through diagnosis and treatment.
It’s big, detailed, and honest…but still human. Think of it as the friend who brings snacks
to your appointment and also happens to read clinical guidelines for fun.
How doctors classify breast cancer: The big picture
Doctors usually sort breast cancer types using three main lenses:
- Where it starts and how far it has spread (in situ vs. invasive).
- How the cells look and grow (ductal, lobular, inflammatory, and other histologic types).
- What fuels the cancer its receptor status (hormone-receptor positive, HER2-positive, or triple-negative).
Most people will hear a combination of these: for example,
“invasive ductal carcinoma, hormone-receptor positive, HER2-negative.” Each piece adds a clue about
which treatments are most likely to work.
Carcinoma in situ: “Stage 0” breast cancer
Ductal carcinoma in situ (DCIS)
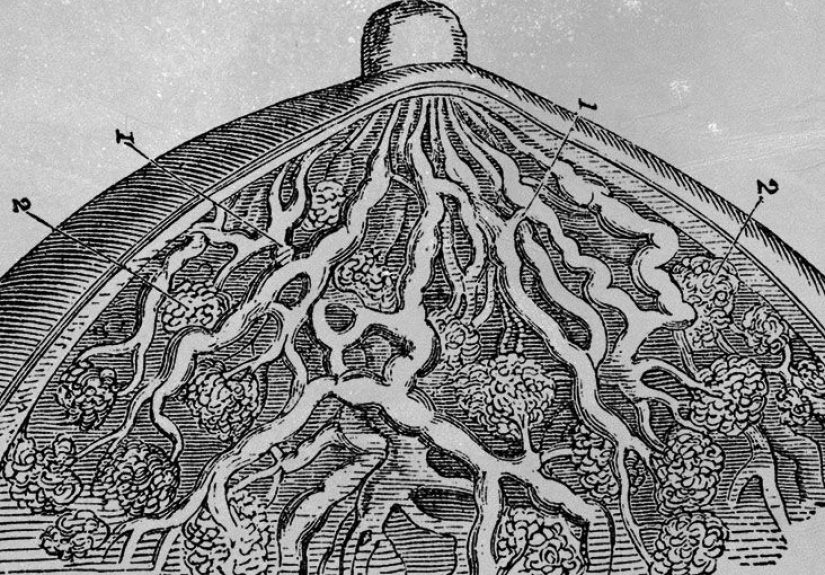
Ductal carcinoma in situ (DCIS) happens when abnormal cells grow inside the milk ducts but have
not broken through the duct wall into surrounding breast tissue. That’s why it’s sometimes called
“non-invasive” or “stage 0” breast cancer.
Key points about DCIS:
- It’s confined to the ducts no invasion into nearby tissue.
- It can sometimes progress to invasive breast cancer over time.
- It’s often found on routine mammograms before symptoms appear.
Symptoms: Many people have no symptoms at all. When symptoms do show up, they may include:
- Abnormal area on a screening mammogram.
- Occasional nipple discharge or a very small lump (less common).
Treatments: Treatment is individualized, but common options include:
- Breast-conserving surgery (lumpectomy) to remove the area of DCIS.
- Radiation therapy after lumpectomy to lower the chance of recurrence.
- Endocrine (hormone) therapy like tamoxifen for hormone-receptor positive DCIS to reduce future risk.
DCIS can feel confusing it’s technically “non-invasive,” but doctors still treat it seriously because it can be a
warning sign of what might come next if it’s ignored.
Lobular carcinoma in situ (LCIS)
Lobular carcinoma in situ (often called LCIS or lobular neoplasia) involves abnormal cells in the
milk-producing glands (lobules). It’s usually considered more of a marker of higher risk than a true cancer.
Key points about LCIS:
- It doesn’t usually show up on mammograms and is often found by accident during a biopsy.
- It raises the lifetime risk of developing invasive breast cancer in either breast.
Treatments and monitoring may include:
- Close imaging follow-up (regular mammograms and sometimes MRI).
- Risk-reducing medications like tamoxifen in some cases.
- Risk-reducing surgery in very high-risk situations (for example, with a strong genetic mutation and family history).
Invasive breast cancers: When cells break out
Invasive (or infiltrating) breast cancers have broken out from ducts or lobules into surrounding breast tissue and
can spread to lymph nodes or distant organs. Most breast cancers diagnosed today are invasive.
Invasive ductal carcinoma (IDC)
Invasive ductal carcinoma (IDC) starts in the lining of a milk duct and then invades nearby breast
tissue. It’s the most common type, making up roughly 70–80% of invasive breast cancers.
Typical symptoms may include:
- A new lump or thickening in the breast or underarm.
- Change in breast size, shape, or contour.
- Skin dimpling, puckering, or a “pulled in” look.
- Nipple changes (turning inward, scaling, discharge).
Common treatments:
- Surgery (lumpectomy or mastectomy) plus evaluation of lymph nodes.
- Radiation therapy after lumpectomy or certain mastectomies.
- Systemic treatments such as chemotherapy, endocrine therapy, and HER2-targeted drugs, depending on receptor status.
Invasive lobular carcinoma (ILC)
Invasive lobular carcinoma (ILC) starts in the lobules (milk-producing glands) and spreads into
surrounding tissue. It is the second most common invasive type.
ILC can be sneaky. Instead of forming one solid lump, it often grows in single-file strands of cells,
which makes it harder to feel on exam and sometimes harder to see clearly on imaging.
Symptoms may be subtle:
- Area of fullness or thickening rather than a distinct lump.
- Changes in breast size or firmness.
- Occasional nipple or skin changes.
Treatment is similar to IDC and usually involves surgery, radiation, and systemic therapies tailored to hormone and HER2 status.
Inflammatory breast cancer (IBC)
Inflammatory breast cancer is a rare but aggressive type where cancer cells block lymph vessels in
the skin of the breast. The breast looks red, swollen, and warm almost like an infection but antibiotics don’t fix it.
Common symptoms:
- Rapid change in one breast over weeks.
- Redness, warmth, or a bruised appearance.
- Skin dimpling or thickening resembling an orange peel (peau d’orange).
- Heaviness, tenderness, or pain.
- Swollen lymph nodes in the armpit or near the collarbone.
Treatment approach:
- Neoadjuvant chemotherapy (chemo given first) to shrink the cancer.
- Surgery, often a mastectomy with lymph node removal if the cancer is still operable.
- Radiation therapy to the chest wall and lymph node regions.
- Endocrine or targeted therapies when the cancer has hormone or HER2 receptors.
Paget disease of the breast
Paget disease of the breast is a rare cancer involving the skin of the nipple and areola. It’s
often associated with an underlying DCIS or invasive cancer deeper in the breast.
Typical symptoms:
- Red, scaly, or crusty nipple skin.
- Itching, burning, or tingling around the nipple.
- Nipple discharge or a flattened nipple.
Because it can look like eczema or dermatitis, Paget disease is sometimes misdiagnosed at first. Persistent
nipple-areola skin changes deserve a careful check by a specialist.
Other less common types
Less common breast cancers include angiosarcoma of the breast, phyllodes tumors,
and certain rare subtypes like mucinous, tubular, or cribriform carcinomas, which often have somewhat more favorable
outcomes.
Male breast cancer is also real, though much less common. Men have breast tissue too, and they can
develop many of the same cancer types, especially invasive ductal carcinoma.
Molecular and receptor types: HR+, HER2+, and triple-negative
Beyond where the cancer started, doctors look at proteins on or inside the cancer cells. These markers guide which
medications are likely to work.
Hormone-receptor positive (HR+)
Many breast cancers are fueled by hormones. If the cells have receptors for estrogen (ER) and/or progesterone (PR),
the cancer is called hormone-receptor positive (HR+).
Why this matters:
- HR+ cancers often grow more slowly.
- They respond well to endocrine therapy (hormone-blocking treatments) like tamoxifen or aromatase inhibitors.
- Endocrine therapy can lower the risk of recurrence for years after treatment ends.
HER2-positive breast cancer
Some breast cancers have extra amounts of a growth-promoting protein called HER2. These are called
HER2-positive breast cancers and make up about 15–20% of cases.
Before modern targeted drugs, HER2-positive cancers tended to be aggressive. Today, medications that directly target
HER2 (such as trastuzumab and others) have dramatically improved outcomes.
Triple-negative breast cancer (TNBC)
Triple-negative breast cancer has none of the three main receptors: no estrogen receptor,
no progesterone receptor, and no HER2 overexpression.
Key features:
- Often more aggressive and more likely to recur in the first few years after diagnosis.
- More common in younger people and some racial/ethnic groups.
- Traditional endocrine and HER2-targeted therapies don’t work because those receptors are missing.
Treatment relies heavily on chemotherapy, and in many cases today, immunotherapy or
newer targeted agents are added, especially for higher-stage disease.
Common symptoms across breast cancer types
Although each type has its quirks, there are shared warning signs. Any of the following should prompt a discussion
with a healthcare professional:
- A new lump, thickening, or area that feels “different” in the breast or underarm.
- Change in breast size, shape, or contour.
- Skin changes (dimpling, scaling, redness, or an orange-peel texture).
- Nipple changes (turning inward, cracking, scaling, or discharge, especially if bloody).
- Persistent breast pain or heaviness that doesn’t line up with your usual cycle.
Many of these symptoms turn out to be benign conditions, but it’s always better to check than to guess. “Watchful
procrastination” is not an official medical strategy.
How treatments are chosen
Treatment is highly personalized. Two people with “the same type” of breast cancer may still have different plans
based on stage, grade, age, other health issues, genetic test results, and personal preferences.
Common treatment building blocks include:
-
Surgery – Lumpectomy (removing just the tumor with a margin of healthy tissue) or mastectomy
(removing the whole breast), often with sampling or removal of lymph nodes. -
Radiation therapy – Uses high-energy beams to kill remaining cancer cells in the breast, chest
wall, or lymph nodes after surgery. -
Systemic therapies – Drugs that travel through the bloodstream:
- Chemotherapy to kill fast-growing cells.
- Endocrine therapy (for HR+ cancers) to block estrogen or lower estrogen levels in the body.
- HER2-targeted therapies for HER2-positive cancers.
- Immunotherapy and newer targeted agents, especially for triple-negative and metastatic disease.
-
Reconstructive and supportive care – Reconstructive surgery, physical therapy for arm mobility and
lymphedema, pain management, mental health support, and survivorship planning.
For some people, treatment starts with surgery; for others, it starts with chemo, endocrine therapy, or targeted
therapy first to shrink the tumor and test how it responds. There isn’t a single “right” sequence there’s the
plan that fits your specific cancer and your life.
Metastatic and recurrent breast cancer
Metastatic breast cancer (also called stage IV) means the cancer has spread to distant organs such
as bone, liver, lungs, or brain. At this stage, the focus shifts from cure to long-term control, symptom relief, and
preserving quality of life for as long as possible.
Recurrent breast cancer is cancer that comes back after treatment in the same breast area,
nearby lymph nodes, or elsewhere in the body. Treatment depends on where it recurs and the cancer’s biology at that
time.
Even in metastatic or recurrent settings, there are more options than ever before, and many people live for years
with well-controlled disease, moving through lines of therapy one step at a time.
Real-life experiences: Navigating breast cancer types in the real world
Medical definitions are important, but they don’t capture what it feels like when a radiology report suddenly
becomes your story. Below are composite, anonymized experiences drawn from common patient narratives not
medical advice, but reflections many people recognize.
“Stage 0” still felt like a very big deal
One woman in her late 40s went in for a routine mammogram and got called back for “additional views.” Her
radiologist saw tiny calcifications and recommended a biopsy. The result: DCIS. No lump, no pain,
no symptoms yet she suddenly found herself talking about surgery and radiation.
Her first reaction was confusion: “If it’s ‘non-invasive,’ why do we have to do anything?” Her team explained that
DCIS is like a fire contained in one room: you can’t assume it will behave and stay there forever. Treating now
dramatically lowers the odds of facing invasive cancer later.
She chose a lumpectomy with radiation and a five-year course of hormone-blocking medication. Side effects were real
(hello hot flashes), but she appreciated having a clear plan and a relatively high chance of long-term control.
When “just dense tissue” turned out to be lobular cancer
Another patient noticed her left breast felt heavier and a bit fuller than the right, but there was no distinct lump.
She was used to her providers blaming everything on “dense breast tissue.” Eventually, she insisted on further
imaging and a targeted ultrasound.
The diagnosis: invasive lobular carcinoma, hormone-receptor positive. In hindsight, she could see
subtle changes in how her bra fit over the previous year, but nothing that screamed “tumor.”
Her experience underscores why it’s important to pay attention not just to lumps, but to changes
asymmetry, fullness, or an area that simply feels “off.” Lobular cancers in particular can be quiet shape-shifters.
Facing triple-negative breast cancer in midlife
A woman in her early 40s found a firm lump in the shower. Within weeks she heard new vocabulary: “triple-negative,”
“neoadjuvant chemo,” and “immunotherapy.” The treatment plan was intense several months of chemotherapy and
immunotherapy before surgery, followed by radiation.
She described treatment as “a second full-time job with lousy benefits,” but she also noticed how much more
coordinated care has become: nurse navigators, nutrition counseling, social workers, and online support communities
that knew exactly what “AC followed by taxol” meant without explanation.
Her biggest takeaway: while triple-negative breast cancer sounded terrifying at first, seeing the tumor shrink on
scans and feeling her doctors’ confidence in the current evidence-based approach helped her move from pure fear
toward cautious optimism.
The emotional side: Waiting, worrying, and re-building
No matter the breast cancer type, certain themes show up again and again:
- The waiting is brutal. Waiting for imaging, biopsies, pathology reports, and treatment plans can feel harder than the treatments themselves.
- Second opinions are normal. People often feel more confident after confirming a plan with a major cancer center or academic hospital.
- Support looks different for everyone. Some share everything on social media; others tell only a tiny circle. There’s no “right” way to cope.
- Identity shifts over time. At first, everything is about being a “patient.” Later, life gradually fills in again work, hobbies, relationships, and long-term survivorship care.
Many survivors describe the experience as learning a new language they never wanted to speak, then becoming the
person others call when they get their own unexpected mammogram results. Knowledge about breast cancer
types DCIS, IDC, ILC, IBC, triple-negative, HER2-positive, hormone-receptor positive becomes not just
vocabulary, but part of a story of resilience.
Important note: This article is for general education only and is not a substitute for professional
medical advice, diagnosis, or treatment. Always consult your healthcare team about your specific situation.