Table of Contents >> Show >> Hide
- Understanding C3G and IgAN: Same Neighborhood, Different Houses
- The Foundation: Supportive Care Still Matters
- Latest Treatments for C3G: Complement Blockers Take the Stage
- Latest Treatments for IgA Nephropathy: From Steroids to Smart Targeted Drugs
- How Doctors Choose a Treatment Plan
- Real-World Experiences: Living Through the New Treatment Era
- Key Takeaways: The Alphabet Soup Is Getting Smarter
Short version: If you’ve ever stared at a lab report that reads like alphabet soupC3G, IgAN, eGFR, UPCRand thought, “Is this a blood test or a Wi-Fi password?”, you are not alone. The good news is that behind all those letters, there has been a quiet revolution in how doctors treat C3 glomerulopathy (C3G) and IgA nephropathy (IgAN). We’ve gone from “supportive care only” to an era of precision medicines, complement inhibitors, and targeted therapies that actually aim at the root of the disease.
This article walks through what C3G and IgAN are, the latest FDA-approved treatments, and how these new options fit into real-life care. It’s information onlynot personal medical adviceso always talk with a nephrologist before making any treatment decisions.
Understanding C3G and IgAN: Same Neighborhood, Different Houses
What is C3 glomerulopathy (C3G)?
C3G is a rare kidney disease where part of your immune systemthe complement system, specifically the alternative pathwaygoes rogue. Instead of calmly helping you fight infections, it stays overactive and deposits complement protein C3 in the filters of the kidneys (the glomeruli). Over time, this can cause inflammation, scarring, protein leaking into the urine (proteinuria), and a gradual loss of kidney function.
Because C3G is rare, many people spend months or years just trying to get the right diagnosis. It typically requires a kidney biopsy with special staining that shows heavy C3 deposits and rules out other causes. For a long time, treatment was basically “best supportive care” and hoping the disease behaved itself. That’s changing fast.
What is IgA nephropathy (IgAN)?
IgA nephropathyoften called Berger’s diseaseis more common. It happens when an antibody called immunoglobulin A (IgA) forms abnormal immune complexes that get stuck in the glomeruli. Those deposits trigger inflammation and, over time, can damage the kidney filters. Classic clues include blood in the urine (sometimes visible, sometimes only on lab tests) and proteinuria.
For years, many people with IgAN heard some version of “We’ll watch your blood pressure and protein and see what happens.” While supportive care is still foundational, we now have multiple medicines that specifically target the pathways driving IgAN instead of just putting a Band-Aid on the symptoms.
Why the complement system matters in both
The complement system is a cascade of proteins that helps your immune system respond quickly to threats. In both C3G and IgAN, the complement system can become overactive. In C3G, complement dysregulation is basically the main villain. In IgAN, it’s more like the villain’s sidekickbut still important.
That’s why so many of the latest treatments for C3G and IgAN are designed to “turn down the volume” on complement activity, with the goal of protecting the kidneys from further damage.
The Foundation: Supportive Care Still Matters
Before we get into shiny new drugs, it’s worth emphasizing that the basics still matter. Even in 2025, almost every treatment plan for C3G or IgAN rests on a common foundation:
- Controlling blood pressure: Usually with ACE inhibitors or ARBs, which also help reduce proteinuria.
- Reducing proteinuria: Beyond ACE/ARB, doctors may add SGLT2 inhibitors or other medicines that have been shown to slow chronic kidney disease progression in many populations.
- Lifestyle support: Low-sodium diet, maintaining a healthy weight, avoiding smoking, and limiting NSAIDsall the un-sexy stuff that actually protects your kidneys long-term.
- Regular monitoring: Lab tests to track proteinuria, eGFR, and blood pressure trends over time, not just one-off snapshots.
Think of supportive care as the “kidney safety net.” New therapies are layered on top of this, not instead of it, especially for people at higher risk of progression.
Latest Treatments for C3G: Complement Blockers Take the Stage
Fabhalta (iptacopan): First FDA-approved treatment for C3G
Until recently, C3G patients had no drug specifically approved for their condition. That changed when the FDA approved Fabhalta (iptacopan), an oral medication that targets factor B, a key protein in the alternative complement pathway. By inhibiting factor B, iptacopan aims to reduce the abnormal C3 activation and deposition that drive C3G.
What makes Fabhalta stand out?
- It’s disease-specific: Approved for adults with C3G to help reduce proteinuria, something patients and doctors have been waiting on for years.
- It’s oral: Taken by mouth, which is a big quality-of-life advantage over frequent IV infusions.
- It targets the root mechanism: Instead of broad immunosuppression, it focuses on complement overactivity.
Clinical trials have shown meaningful reductions in proteinuria and promising trends in preserving kidney function. That said, complement inhibition can raise infection risksespecially from certain bacteriaso vaccination and infection-prevention strategies are a key part of care.
Other complement inhibitors in C3G research
Fabhalta is the first approved drug, but it’s unlikely to be the last. A number of other complement-targeting medicines are under investigation for C3G, including:
- C3 inhibitors (such as pegcetacoplan), which act a bit further down the cascade.
- Monoclonal antibodies against complement components (for example, drugs related to eculizumab or ravulizumab), initially developed for conditions like atypical HUS and PNH.
- C5a receptor blockers such as avacopan, being studied in select complement-driven kidney diseases.
These drugs differ in route (IV vs. subcutaneous vs. oral), dosing frequency, and which rung on the complement ladder they target. That means future treatment may be much more personalized: some people might do best with a proximal blocker like iptacopan, others with a different mechanism based on genetics, biopsy findings, or prior response.
Clinical trials and who might be eligible
Because C3G is rare, clinical trials are especially important. Typical eligibility factors include age, biopsy-confirmed C3G, a certain level of proteinuria, and an eGFR above a defined threshold. Some trials accept people with kidney transplants, others don’t. If someone has C3G and is still losing kidney function despite supportive care, asking their nephrologist about ongoing trials can be a very reasonable step.
As always, trials come with trade-offs: extra visits, lab work, and unknowns about long-term outcomes. But for some patients, they offer access to therapies years before they become widely available.
Latest Treatments for IgA Nephropathy: From Steroids to Smart Targeted Drugs
Tarpeyo (budesonide delayed release): A gut-targeted steroid
Tarpeyo is an oral, delayed-release form of budesonide designed to deliver high steroid concentrations to the area of the small intestine where much of the abnormal IgA production may start. The idea is elegant: hit the problem closer to its origin while limiting whole-body steroid exposure.
Tarpeyo is approved to reduce the loss of kidney function in adults with primary IgAN who are at risk for disease progression. In clinical studies, it reduced proteinuria and showed benefits in preserving eGFR over time. Because it is still a corticosteroid, side effects such as weight gain, elevated blood pressure, mood changes, or blood sugar issues remain possible, but the targeted delivery may lessen the systemic burden compared with conventional oral steroids.
Sparsentan (Filspari) and other endothelin receptor antagonists
Sparsentan (Filspari) is a dual endothelin type A and angiotensin II receptor blocker. That’s a long way of saying it blocks two pathways involved in kidney damage and blood pressure regulation. Initially granted accelerated approval, sparsentan later received full FDA approval for IgAN based on long-term data showing greater preservation of kidney function compared with irbesartan in a head-to-head trial.
Key points about sparsentan:
- Non-immunosuppressive: It works through hemodynamic and signaling pathways rather than damping down the entire immune system.
- Proteinuria reduction: It can significantly reduce protein loss in the urine, a major predictor of future kidney function.
- Monitoring: Because endothelin receptor antagonists can affect liver function and fluid status, lab checks and blood pressure/weight monitoring are part of the picture.
Another endothelin receptor antagonist, Vanrafia (atrasentan), has also entered the IgAN scene with accelerated approval, adding more options in this class. That’s good news for patients and slightly stressful news for insurers.
Biologics and complement-targeted therapies for IgAN
If C3G led the way in complement therapy, IgAN is quickly catching up. Several new and emerging options include:
- Voyxact: A monoclonal antibody approved to reduce proteinuria in adults with primary IgAN. It is given by injection about once every four weeks, with the convenience of potential at-home administration in many cases.
- Complement inhibitors: Drugs that target components of the alternative or terminal complement pathways are being tested in IgAN, including versions of iptacopan and other agents first explored in C3G.
- B-cell– and IgA-targeting biologics: Agents like atacicept and others under investigation aim to reduce the abnormal IgA production at its source by modulating B cells and plasma cells.
These medicines are not “starter drugs.” They are typically reserved for patients at higher risk of progressionoften those with persistent proteinuria despite optimized supportive care and sometimes after or instead of systemic steroids, depending on the individual situation and evolving guidelines.
Where SGLT2 inhibitors and classic therapies fit
While they aren’t specific to C3G or IgAN, SGLT2 inhibitors (like empagliflozin and dapagliflozin) have become key players in chronic kidney disease management overall. Many nephrologists now consider them part of the backbone therapy for eligible patients with proteinuric kidney disease, regardless of whether diabetes is present.
These drugs, combined with ACE inhibitors or ARBs, form the “boring but powerful” base layer. Newer agents like Tarpeyo, sparsentan, Voyxact, or complement inhibitors are then added for people who remain at risk of progression despite best standard care.
How Doctors Choose a Treatment Plan
If you were hoping for a tidy flowchart like “If C3G, then pill A; if IgAN, then pill B,” sorryreal-world nephrology is more nuanced. Treatment decisions usually consider:
- Diagnosis and biopsy findings: Is it C3G, IgAN, or a related complement-mediated disease? How much scarring is already present?
- Risk of progression: Level of proteinuria, eGFR trend, blood pressure control, and prior treatment response all matter.
- Comorbidities and preferences: Conditions like diabetes, liver disease, pregnancy plans, and willingness to come in for infusions or frequent labs can tilt the choice toward one drug over another.
- Side-effect profile: Some patients might accept steroid-related side effects but want to avoid liver monitoring; others may prefer biologics over oral steroids, or vice versa.
- Insurance and access: Unfortunately, coverage, co-pays, and prior authorization requirements often influence which “latest and greatest” drug is realistically available.
Most people end up with a layered plan: optimized blood pressure management, possibly an SGLT2 inhibitor, plus one or more disease-specific agents like Tarpeyo, sparsentan, Voyxact, or a complement inhibitoralways individualized and adjusted over time.
Important disclaimer: None of these medicines should be started, stopped, or changed without direct guidance from a kidney specialist who knows the patient’s full medical history.
Real-World Experiences: Living Through the New Treatment Era
Statistics and acronyms are nice, but they don’t show what it actually feels like to live with C3G or IgAN while navigating all these new options. The following are composite examplesbased on common patient experiencesnot real individuals, but they illustrate what this new treatment era can look like.
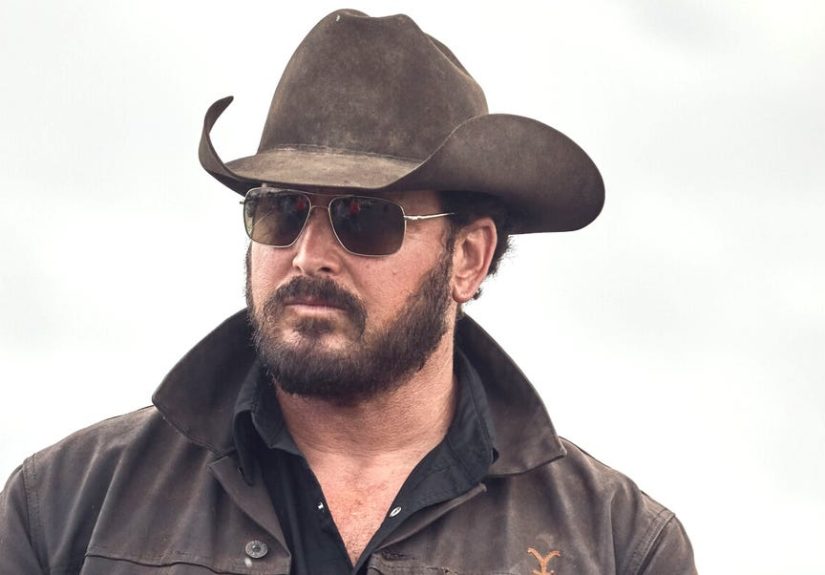
“Maria,” 32, with IgAN and a busy life
Maria is in her early thirties, works full-time, and has two small kids who think 6 a.m. is a perfectly reasonable wake-up time. After years of microscopic hematuria, she finally had a kidney biopsy that confirmed IgAN. Her blood pressure is well-controlled on an ARB, but her proteinuria stayed stubbornly high.
Her nephrologist added an SGLT2 inhibitor first. Proteinuria dropped, but not enough. After a detailed discussion of risks, benefits, and monitoring, they decided to start a targeted therapysparsentan. Maria had to repeat labs more often at first and adjust her schedule for follow-ups, but over the next year her protein levels dropped, and her eGFR stabilized. She still checks her blood pressure at home and reads labels for sodium, but she also has more emotional bandwidth to focus on life outside the lab portal.
“Devin,” 19, with C3G starting university
Devin was diagnosed with C3G as a teenager after he developed swelling and foamy urine. For a while, his treatment plan was “good blood pressure control, low-salt diet, and let’s hope.” As he prepared to leave for college, his proteinuria started climbing again, and his nephrologist worried about accelerated kidney damage.
With the approval of iptacopan, Devin had an option that didn’t exist just a few years earlier. After counseling about infection risks and vaccination, he started the medication. Over months, his proteinuria decreased and stabilized. He still goes for regular lab work, but he can take his medicine orally at school without needing frequent infusions. For a college student juggling exams, laundry, and the mystery of communal refrigerators, that’s a big deal.
What patients often say matters most
Across many stories, a few themes keep showing up:
- Feeling heard: Patients appreciate when doctors take time to explain what each drug does and why it’s being considerednot just “because the guideline says so.”
- Clear expectations: Knowing up front about lab work, possible side effects, and what counts as an emergency helps people feel in control.
- Shared decision-making: Many patients want to be partners, not passengers. They may choose one drug over another based on lifestyle, family plans, or risk tolerance.
- Support networks: Connecting with patient organizations or online communities specific to IgAN or C3G can make the journey less isolating and provide practical tips for day-to-day life.
New drugs can’t remove all the uncertainty of living with a chronic kidney disease, but they can shift the story from “inevitable decline” to “there are tools we can use.” For many people, that’s an enormous psychological turning point.
Key Takeaways: The Alphabet Soup Is Getting Smarter
- C3G and IgAN are immune-mediated kidney diseases that often involve an overactive complement system and can lead to progressive loss of kidney function.
- Supportive care remains essentialblood pressure control, RAAS blockade, SGLT2 inhibitors when appropriate, and lifestyle measures are still the base of therapy.
- For C3G, Fabhalta (iptacopan) is now the first FDA-approved, disease-specific treatment, with other complement inhibitors in the pipeline.
- For IgAN, Tarpeyo, sparsentan, Voyxact, and other targeted agents offer options beyond traditional steroids and generic blood pressure drugs, especially for patients at higher risk of progression.
- Treatment is highly individualized: the “right” regimen depends on biopsy findings, risk profile, comorbidities, and patient preferences.
- Talk to a nephrologist: Online articles are a great starting point, but actual treatment decisions must be made with a kidney specialist who knows the full clinical picture.
We’re still early in this new era, but for people living with C3G or IgAN, it’s the difference between watching the storm roll in and finally having a better umbrella.