Table of Contents >> Show >> Hide
- What Does “500% Increase” Actually Mean?
- Where the “500%” Number Comes From (and Why That Matters)
- Why Doctors Are Taking This Seriously, Even Though It’s Still Rare
- Symptoms Parents and Teens Shouldn’t Brush Off
- Who Is Most at Risk? The Short (But Important) List
- So Why Are Rates Rising? The Leading Theories (and the Honest Truth)
- Why Screening Guidelines Changed for Adultsbut Not for Kids
- What Parents Can Do (That Actually Helps)
- What Happens If a Doctor Is Concerned?
- FAQ: Quick Answers to Common (and Very Human) Questions
- Bottom Line
- Real-World Experiences: What the “500%” Looks Like in Life (Not Just a Graph)
If you just did a double-take at that headline, good. You’re supposed to.
“Colorectal cancer” is a phrase most of us file under “stuff I’ll worry about when I’m older,” somewhere between
knee noises and reading glasses. But U.S. data presented in recent years has put a spotlight on an uncomfortable
reality: colorectal cancer (CRC) is rising in younger peopleincluding kids and teens.
Before anyone panic-buys kale and cancels birthday cake: colorectal cancer in children is still rare.
The number that’s getting attention“500% increase in ages 10–14”is a relative jump from a very low baseline.
It’s still alarming, but it’s also easy to misunderstand. Let’s break down what the statistic means, why doctors care,
what symptoms families shouldn’t ignore, and what practical prevention and risk-reduction looks like in real life.
What Does “500% Increase” Actually Mean?
“500% increase” sounds like a tidal wave. In reality, it’s more like a small puddle becoming a bigger puddle
and doctors are worried because puddles shouldn’t be growing where puddles historically didn’t exist.
In the analysis widely reported from U.S. surveillance data (1999–2020), the incidence rate of colorectal cancer
in children aged 10 to 14 rose from about 0.1 per 100,000 in 1999 to about 0.6 per 100,000 in 2020.
That’s a 500% relative increaseyet it’s still fewer than 1 case per 100,000 kids in that age group.
| Age group | 1999 rate (per 100,000) | 2020 rate (per 100,000) | Relative change |
|---|---|---|---|
| 10–14 | 0.1 | 0.6 | +500% |
| 15–19 | 0.3 | 1.3 | +333% |
| 20–24 | 0.7 | 2.0 | +185% |
So yes, the growth is real. But the bigger story isn’t that colorectal cancer is suddenly common in middle schoolers.
It’s that the trend line is moving the wrong way in multiple younger age groups, and we don’t have one neat explanation.
Where the “500%” Number Comes From (and Why That Matters)
The “500%” figure comes from a multi-decade look at U.S. cancer incidence trends using large public health datasets
(reported via CDC surveillance tools and presented in a major gastroenterology meeting context). That’s important because:
- It’s population-level data, not a single hospital’s experience.
- It measures rates over time, not the personal risk of any one child.
- It raises a hypothesis (“something is changing”) but does not prove a single cause.
In other words: it’s a warning light on the dashboard, not a complete engine diagnosis.
Why Doctors Are Taking This Seriously, Even Though It’s Still Rare
Colorectal cancer in kids and teens creates a perfect storm:
low awareness + symptoms that overlap with common issues + delays in diagnosis.
And when CRC is found in younger people, it’s often discovered later than anyone would like.
Meanwhile, broader U.S. trends show colorectal cancer has become an increasingly significant cause of cancer death
in people under 50enough that major organizations emphasize both symptom education and appropriate screening for adults.
(Kids are not routinely screened, but adults are now generally advised to start average-risk screening earlier than in the past.)
Translation: the medical community is not saying “every child needs a colonoscopy.”
It is saying “don’t dismiss persistent red flags just because someone is young.”
Symptoms Parents and Teens Shouldn’t Brush Off
Most bowel changes in kids are not cancer. They’re constipation, stomach bugs, lactose intolerance, stress, or “I ate three
frosting-heavy cupcakes and now my body is writing a complaint letter.” Still, certain symptoms deserve attentionespecially
if persistent, worsening, or unexplained.
Common red-flag symptoms reported in younger CRC cases
- Blood in or on the stool (or rectal bleeding)
- Persistent change in bowel habits (new constipation, diarrhea, narrower stools, or “never feels finished”)
- Ongoing abdominal pain or cramping that doesn’t settle
- Unexplained weight loss or appetite changes
- Iron-deficiency anemia (fatigue, pallor, shortness of breath, dizziness)
If you’re thinking, “But hemorrhoids can cause bleeding,” you’re right. So can fissures. So can inflammatory bowel disease.
The point isn’t to self-diagnoseit’s to get evaluated when symptoms persist or stack up.
Who Is Most at Risk? The Short (But Important) List
Childhood and teen CRC is uncommon, and when it happens, clinicians pay close attention to risk factors that can push the odds
upward. Some are inherited, some are medical-history related, and some are lifestyle-linked (though lifestyle alone doesn’t
explain everything).
Higher-risk groups include
- Family history of colorectal cancer or advanced polyps, especially in a close relative and especially at younger ages
- Hereditary cancer syndromes (e.g., Lynch syndrome, familial adenomatous polyposis/FAP, and other polyposis syndromes)
- Inflammatory bowel disease (IBD), particularly long-standing ulcerative colitis or Crohn’s disease involving the colon
- Prior abdominal/pelvic radiation for another condition (in certain scenarios)
If your family has a known inherited syndrome, the strategy is different: surveillance can start earlier, and care is usually guided
by genetics specialists and gastroenterology teams. That’s not alarmismit’s precision.
So Why Are Rates Rising? The Leading Theories (and the Honest Truth)
Here’s the part everyone wants: one clear culprit. Unfortunately, early-onset colorectal cancer appears to be a
multi-factor story. Researchers suspect a combination of changes in environment, metabolism, diet patterns, physical activity,
and gut biologyplus genetics and chance.
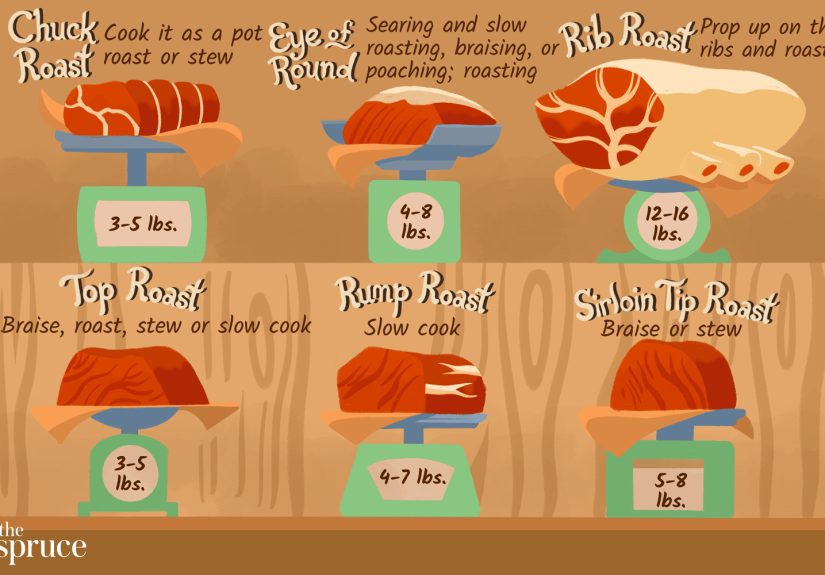
1) Diet patterns and metabolic health
Over the last few decades, many Americans have shifted toward diets higher in ultra-processed foods and lower in fiber.
At a population level, obesity and metabolic dysfunction have also increased. These factors are associated with colorectal cancer risk in adults,
and they’re frequently discussed as contributors to rising early-onset CRC.
Important nuance: plenty of people with “good” diets still develop CRC, and plenty of people with “bad” diets never do.
Risk isn’t destiny. But public health trends can still matter.
2) Sedentary time
Sitting isn’t a moral failingit’s what school and modern work demand. But higher sedentary time is often mentioned alongside diet and obesity
in CRC risk discussions. Movement helps regulate inflammation, insulin sensitivity, and gut motility (your colon loves a walk more than it loves
your group chat).
3) Microbiome shifts, antibiotics, and a toxin called colibactin
One of the most talked-about research angles recently involves colibactin, a toxin produced by certain strains of
E. coli. A major study published in Nature reported that mutations linked to colibactin exposure were substantially more common
in early-onset colorectal cancers, suggesting early-life exposures could play a role.
This doesn’t mean “E. coli causes colon cancer” in a simple way. It means researchers are tracking how early microbial exposures might leave long-term
DNA “footprints” thatalong with other factorscould raise risk. It’s a fast-moving area of science, and it’s not a reason to panic.
It is a reason to fund research and take symptoms seriously.
4) The “cohort effect” idea
National cancer experts have described a pattern where risk appears higher in more recent birth cohortssuggesting something about the modern environment,
especially early-life exposures, could be influencing cancer risk later on. This idea is being explored across several early-onset cancers, not just CRC.
Why Screening Guidelines Changed for Adultsbut Not for Kids
You may have heard that colorectal cancer screening now starts earlier. That’s true for average-risk adults:
major U.S. groups recommend starting routine screening at age 45 for adults at average risk.
But kids are a different situation. The incidence in children is still extremely low, and the risks and burdens of widespread colonoscopy screening
would outweigh potential benefits at the population level.
For children and teens, the most practical approach is:
risk-based evaluation (family history, genetic syndromes, IBD) plus symptom-based action
(don’t ignore persistent red flags).
What Parents Can Do (That Actually Helps)
If you’re a parent reading this and feeling the urge to wrap your child in bubble wrap and feed them nothing but blueberries:
I get it. But the best actions are boringin the good way.
1) Treat rectal bleeding as “check it,” not “shhh, it’s embarrassing”
Embarrassment is a powerful force. It convinces teens to hide symptoms and convinces adults to assume it’s “probably nothing.”
Create a household culture where poop is medically normal to talk about. Not at the dinner table. But normal.
2) Know your family history
If close relatives had colorectal cancer or lots of polypsespecially at younger agesshare that information with your child’s clinician.
It can change the threshold for referrals, genetic counseling, and surveillance planning.
3) Build a gut-friendly routine (without turning meals into a punishment)
- Fiber forward: fruits, vegetables, beans, whole grainswork up slowly if your kid is fiber-shy
- Limit processed meats and frequent sugar-sweetened drinks
- Move most days: sports, walking, dancing, bikingwhatever gets them happily un-stationary
- Sleep and stress: not glamorous, but huge for overall health patterns
None of this guarantees prevention. It’s about shifting odds in the right direction and supporting overall health.
What Happens If a Doctor Is Concerned?
Evaluation depends on symptoms and risk. The clinician may:
- Take a detailed history (including family history, IBD symptoms, weight changes)
- Order labs (especially for anemia or inflammation markers)
- Consider stool tests (to evaluate bleeding or inflammation, depending on context)
- Refer to pediatric gastroenterology
- In higher-concern scenarios, recommend imaging and/or colonoscopy
If colorectal cancer is diagnosed (again, rare), treatment is typically handled by a specialized team and may include surgery,
chemotherapy, radiation (especially for rectal tumors), andin select casestargeted therapy or immunotherapy depending on tumor features.
FAQ: Quick Answers to Common (and Very Human) Questions
Is colorectal cancer really becoming common in children?
No. It remains rare. The concern is the upward trend in rates over time, not that most kids are at high risk.
Should my 12-year-old get screened?
Routine screening for average-risk children isn’t recommended. But evaluation is appropriate if there are persistent symptoms
(especially bleeding, anemia, or significant bowel changes) or high-risk medical/family history.
My teen has stomach pain and constipation. Should I assume the worst?
Nothose symptoms have many common causes. But if symptoms are persistent, worsening, or paired with red flags (blood, weight loss, anemia),
it’s worth a medical visit rather than a “let’s wait another month” strategy.
Bottom Line
The “500% increase” headline is both attention-grabbing and incomplete without context. The clearest, most responsible takeaway is this:
colorectal cancer in children is still rare, but rates in younger age groups have risen over timeand persistent red-flag symptoms deserve evaluation.
We don’t yet have a single proven explanation for why early-onset colorectal cancer is increasing. Researchers are investigating lifestyle patterns,
metabolic health, environmental and microbiome shifts, and intriguing new science (like colibactin-related DNA signatures). While we wait for clearer answers,
families can focus on realistic prevention habits and, crucially, on not ignoring symptoms just because someone is young.
Real-World Experiences: What the “500%” Looks Like in Life (Not Just a Graph)
Numbers are clean. Life isn’t. What follows are composite experiencesbuilt from common themes reported by clinicians, public health messaging,
and patient education narrativesmeant to capture what families often describe when a rare diagnosis collides with ordinary routines.
Experience #1: “It was probably hemorrhoids… until it wasn’t.”
A middle-schooler mentions blood when wiping. A parent assumes constipation or a fissure. The symptoms come and go, and because kids are busy being kids,
nobody wants to turn bathroom talk into a family meeting. Months later, fatigue shows upquietly at first. The child stops wanting to run around at recess.
A school nurse notes they look pale. A simple blood test reveals iron-deficiency anemia. That’s often the moment the story changes from “probably nothing”
to “let’s investigate.” Even then, families describe surprise at how long it can take to connect the dotsbecause the early symptoms overlap with so many
benign issues.
Experience #2: The “stomach ache” that becomes a calendar event.
Abdominal pain is practically a childhood rite of passage. It can be stress, food intolerance, viral illness, constipation, or a dozen other things.
What tends to raise concern is pattern: pain that keeps returning, pain that worsens, pain with bowel changes, pain with weight loss, or pain with
visible bleeding. Families often say the turning point wasn’t a single symptomit was the repetition. “It kept happening,” they’ll report, “and it stopped
responding to the usual fixes.” Clinicians frequently emphasize that persistence matters: a symptom that refuses to leave deserves a second look.
Experience #3: The teen who didn’t want to be “dramatic.”
Teens are experts at minimizing things that make them feel different. Some report hiding rectal bleeding because it’s embarrassing. Others normalize
bowel changes because “my stomach is always weird.” When diagnosis is delayed, families often say it wasn’t because they didn’t careit was because nobody
imagined colorectal cancer belonged in the teen years. The lesson many share afterward is deceptively simple: if a symptom feels wrong and keeps coming back,
it’s not “dramatic” to ask for help.
Experience #4: The family history surprise.
Sometimes a diagnosis triggers a cascade of revelations: “Grandpa had colon cancer at 52,” or “Aunt had tons of polyps,” or “We always thought it was
random.” Genetic counseling can feel intimidating, but families often describe it as clarifyingespecially when it identifies a hereditary syndrome that
explains why cancer showed up early. In those scenarios, the diagnosis is still painful, but the path forward becomes more structured: relatives can be tested,
surveillance plans can be made, and future risk can be managed with something better than guesswork.
Experience #5: The practical aftermathschool, sports, and normal life.
When a child is undergoing evaluation (or treatment), the day-to-day becomes the real battleground: missed classes, scheduling appointments, managing fatigue,
handling dietary changes, and the emotional weight of uncertainty. Families often say they needed two kinds of support: medical expertise and plain logistics
helprides, meals, tutoring plans, and someone to sit with siblings. That’s why awareness matters: early evaluation doesn’t just affect medical outcomes; it can
reduce the length of time families live in the stressful limbo of “What is happening?”
These experiences don’t mean the average child is in danger. They do mean this: the most actionable response to the “500%” headline isn’t panicit’s
attention. Attention to persistent symptoms. Attention to family history. Attention to healthy routines that support long-term risk reduction.
And attention to the fact that colorectal cancer is no longer a topic reserved for retirement-age conversations.