Table of Contents >> Show >> Hide
- Why Heart Failure Hits Black and Hispanic Communities Harder
- Heart-Healthy Eating: Foundations Before the Fine Print
- Eating Well When Access and Cost Get in the Way
- Exercise and Heart Failure: Moving Safely, Not Perfectly
- Making Lifestyle Change Culturally Relevant
- Partnering With Your Care Team
- Real-Life Experiences: How People Are Putting This Into Practice
- Putting It All Together
Getting told you have heart failure can feel like your heart’s warranty just expired. For many
Black and Hispanic families, that news also lands on top of long workdays, tight budgets,
and cultural traditions that absolutely involve food. The good news: what you eat and how
you move still makes a powerful difference, even after a heart failure diagnosis and those
changes can be tailored to your culture, your schedule, and your reality.
In this guide, we’ll walk through how diet and exercise help manage heart failure, why Black
and Hispanic communities face higher risks, and practical ways to make lifestyle changes
that respect beloved foods and family routines. Think of it as a heart-health playbook you can
actually use, not a list of “never eat this again” rules.
Why Heart Failure Hits Black and Hispanic Communities Harder
Heart failure happens when the heart can’t pump blood as well as it should. It doesn’t mean
your heart stops working; it means it’s struggling to keep up with your body’s needs.
Studies show that Black and Hispanic adults in the United States are more likely to develop
heart failure, often at younger ages, and face higher rates of hospitalizations and worse
outcomes than White adults.
Several factors drive these disparities:
- Higher rates of risk factors: High blood pressure, diabetes, and obesity are more common in many Black and Hispanic communities, and all strongly increase heart failure risk.
- Unequal access to care: Black and Hispanic patients are less likely to receive advanced heart failure therapies like cardiac devices, ventricular assist devices, or transplants, even when medically eligible.
- Social and economic pressures: Food deserts, lack of safe places to exercise, language barriers, transportation issues, and limited insurance coverage all make “just eat better and move more” much harder than it sounds.
Diet and exercise can’t fix systemic inequities, but they can help people with heart failure
feel better, stay out of the hospital more often, and live fuller lives.
Heart-Healthy Eating: Foundations Before the Fine Print
The Big Picture: What Your Heart Loves
Whether your favorite dishes are rice and beans, collard greens, plantains, or tamales, the
core of a “heart failure diet” lines up with general heart-healthy nutrition guidelines:
- Plenty of fruits and vegetables of all colors (fresh, frozen, or canned in water).
- Whole grains like brown rice, oats, barley, and whole wheat tortillas.
- Lean protein from beans, lentils, peas, skinless poultry, fish, and small portions of lean meats.
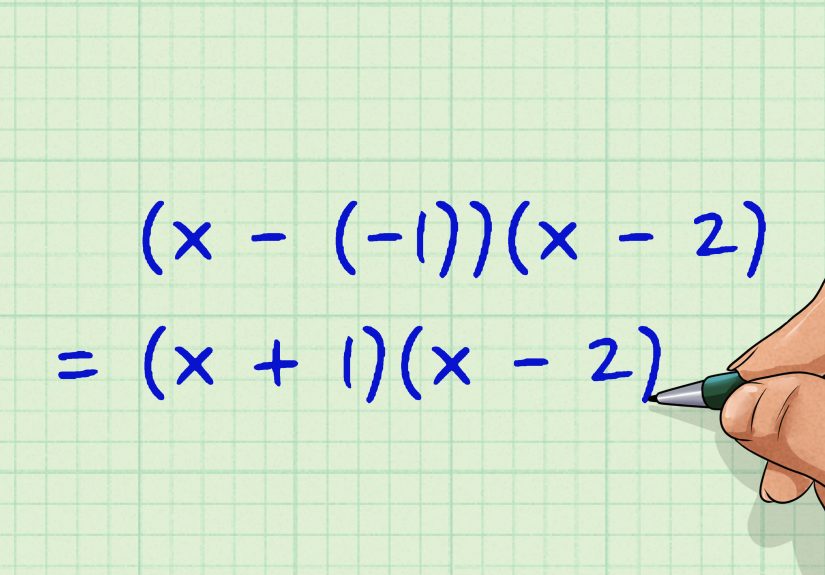
- Healthy fats from olive oil, canola oil, nuts, seeds, and avocado instead of butter or lard.
- Limited added sugars and ultra-processed foods, especially sugary drinks and packaged snacks.
Many of these ideas overlap with the DASH (Dietary Approaches to Stop Hypertension) eating
pattern, which emphasizes fruits, vegetables, whole grains, and low-fat dairy and has been
linked to lower blood pressure and a reduced risk of heart failure.
Sodium: The Sneaky Trouble-Maker
In heart failure, your body tends to hold on to fluid. Sodium (salt) acts like a magnet that
pulls water into your bloodstream and tissues. Too much sodium can worsen swelling in your
legs, belly, and lungs, making you feel more short of breath and uncomfortable.
Many heart failure care teams recommend limiting sodium to around 1,500–2,000 milligrams per day
less than a teaspoon of salt though the exact target should be personalized with your
clinician because very strict limits may not be right for everyone.
Helpful sodium-saving habits include:
- Checking food labels and choosing “low-sodium” or “no salt added” versions when possible.
- Rinsing canned beans and vegetables under water to wash away some of the salt.
- Flavoring food with herbs, spices, garlic, citrus, onion, and pepper instead of reaching for the salt shaker.
- Watching out for restaurant meals, bouillon cubes, seasoning packets, instant noodles, and salty snacks they’re often salt bombs in disguise.
If your doctor has also given you a fluid restriction (for example, limiting total drinks per day),
make sure to balance that with hot weather, sweating, or heavy exercise. Never change fluid
or sodium targets without checking in with your care team.
Keeping the Flavor in Cultural Foods
Heart-healthy eating does not mean abandoning your culture’s dishes. It means nudging
recipes in a more heart-friendly direction:
- Black and Afro-Caribbean cuisines: Keep the collard greens, but cook them with smoked turkey instead of salt pork; flavor rice and peas with herbs, onions, and low-sodium broth. Bake or grill jerk chicken instead of frying it, and trim visible fat.
- Mexican and Central American dishes: Choose corn tortillas over fried shells, load up on pico de gallo, salsa, beans, and grilled meats, and keep cheese, sour cream, and salty chips in smaller portions. Make pozole or caldo with more veggies and less salty broth.
- Puerto Rican, Dominican, and Cuban traditions: Use more herbs, garlic, onion, and vinegar and less sofrito cubes or bouillon. Try baking plantains instead of frying, and replace part of the white rice with brown rice or quinoa.
The goal is to keep the soul of your food the flavors and family memories while quietly
cutting back on salt, saturated fat, and heavy frying.
Eating Well When Access and Cost Get in the Way
It’s easy to say “eat fresh produce and wild salmon” when you live near a big supermarket and
have a flexible budget. Many Black and Hispanic neighborhoods don’t have that luxury. That’s
why realistic heart failure diet advice has to work in the real world.
Some practical strategies:
- Use frozen and canned smartly: Frozen fruits and veggies are often cheaper and just as nutritious. Canned beans and vegetables can be fine if you choose low-sodium or rinse them well.
- Buy in bulk and batch cook: Big bags of brown rice, oats, and dried beans are relatively affordable and stretch across many meals.
- Shop the sales: Look for deals on chicken thighs, turkey, or fish, and freeze portions.
- Leverage community resources: Food pantries, senior meal programs, church food distributions, and community health workers can help bridge gaps.
- Plan around what’s available: Instead of planning a perfect menu and getting frustrated, look at what’s in your local store and build balanced meals from there.
If you qualify for SNAP or similar programs, ask your clinic or hospital social worker to
connect you with applications or local organizations that can walk you through the process.
Exercise and Heart Failure: Moving Safely, Not Perfectly
Exercise might sound risky when your heart already seems overwhelmed, but regular physical
activity is actually one of the best tools for improving exercise tolerance, mood, and
day-to-day function in heart failure.
For most adults, including those with heart disease, the American Heart Association suggests
aiming for about 150 minutes of moderate-intensity aerobic activity per week things like
brisk walking plus muscle-strengthening activities on at least two days per week.
In heart failure, this is usually a long-term goal, not a starting point.
Best Types of Exercise for Heart Failure
Your exact exercise prescription should come from your healthcare team or a cardiac rehab
program, but common options include:
- Walking: The classic. Start with 5–10 minutes at an easy pace and add 1–2 minutes every few days as tolerated, aiming toward 30–45 minutes on most days.
- Cycling or stationary biking: Good if walking bothers your joints.
- Light strength training: Using light weights or resistance bands can improve muscle strength and make daily tasks (stairs, carrying groceries) easier.
- Chair exercises: For people with limited mobility, seated marches, arm raises, and gentle stretches still count.
- Everyday movement: Short bursts of effort climbing stairs, walking to the bus stop, dancing in the living room can also support heart health, especially when done consistently.
Safety Rules You Shouldn’t Skip
For people with heart failure, the rules around exercise include:
- Get cleared first: Always talk to your cardiologist or primary care provider before starting or changing an exercise plan.
- Warm up and cool down: Spend at least 5–10 minutes easing into activity and another 5–10 minutes easing out.
- Use the “talk test”: During moderate activity, you should be able to talk but not sing. If you can’t speak in full sentences, you’re likely overdoing it.
- Listen to symptoms: Stop exercising and seek medical advice if you have chest pain, severe shortness of breath, dizziness, or new palpitations.
- Watch your weight and swelling: Sudden weight gain, more ankle swelling, or worsening shortness of breath may mean your heart failure is flaring and your exercise plan needs adjustment.
Many people with heart failure benefit from cardiac rehabilitation, a structured program
where exercise, education, and support are supervised by a health care team. Ask your
provider if you qualify and whether there are programs near your home, community center, or
trusted local hospital.
Making Lifestyle Change Culturally Relevant
Diet and exercise advice works best when it fits your life, language, and traditions. For Black
and Hispanic communities, that often means:
- Involving family: If one person has heart failure but everyone still wants fried food and giant portions, it’s going to be tough. Shifting recipes and routines together spreads the benefits and the effort.
- Tapping into community spaces: Faith communities, barbershops, beauty salons, community centers, and block associations can all be powerful hubs for walking groups, cooking classes, and health talks.
- Using Spanish-language or culturally tailored materials: Ask for handouts or apps in your preferred language, and don’t hesitate to request an interpreter at medical visits.
- Respecting traditions while editing recipes: Instead of banning a favorite holiday dish, experiment with lower-sodium seasoning, more veggies, or smaller portions.
Heart failure management doesn’t have to erase cultural identity. It can, instead, update
family habits so that future generations inherit more recipes and more healthy years.
Partnering With Your Care Team
Because heart failure is complex, diet and exercise choices should be coordinated with your
health care team. Before you make big changes, consider asking:
- “What is my sodium and fluid goal?”
- “Which kinds of exercise are safe for me, and how should I start?”
- “Can you refer me to a cardiac rehab program?”
- “Can I meet with a registered dietitian who understands my cultural foods?”
- “Are there programs that help with food or transportation?”
If something your doctor says doesn’t make sense, ask for clarification. You are the expert
on your own life; they are the expert on heart failure. You need both sets of expertise to
build a plan that works.
Real-Life Experiences: How People Are Putting This Into Practice
The stories below are composites inspired by real-world experiences from patients, families,
and clinicians. They’re not any one person’s medical record, but they reflect common
challenges and creative solutions in Black and Hispanic communities managing heart failure
with diet and exercise.
Ms. J’s Sunday Dinner Makeover
Ms. J is a 62-year-old Black grandmother who loves hosting Sunday dinners. When she was
hospitalized with heart failure, the discharge instructions looked like a personal attack on
her menu: fried chicken, macaroni and cheese, greens simmered with ham hocks, cornbread
all on the “go easy” or “avoid” list because of sodium and saturated fat.
At first, she tried cooking a separate “healthy” meal for herself. She lasted exactly two
Sundays before giving up and sliding back into old habits. The turning point came when her
daughter joined a session with the clinic dietitian. Together, they worked out small changes
that kept the soul of the meal:
- Oven-“fried” chicken coated in seasoned breadcrumbs and baked on a rack.
- Collard greens cooked with smoked turkey and extra onion, garlic, and red pepper flakes instead of salted pork.
- Half the macaroni and cheese swapped for baked cauliflower in a lighter cheese sauce.
- Fresh fruit salad for dessert instead of store-bought pies.
It wasn’t perfect no one is weighing out the sodium content of every spoonful but Ms. J
noticed less bloating and fewer “I can’t catch my breath” days. Her grandkids still cleaned
their plates. The dietitian called that a win.
Carlos’ Truck-Stop Strategy
Carlos is a 48-year-old Puerto Rican truck driver with heart failure and diabetes. His life is
basically highways and gas stations. Telling him to “cook fresh meals at home and eat more
salads” was… not helpful.
With his cardiology nurse, he made a custom “truck-stop game plan”:
- At fast-food places, choose grilled chicken sandwiches without cheese or mayo, skip the fries, and order water.
- From convenience stores, pick low-sodium nuts, fruit cups in juice (drained), hard-boiled eggs, and low-sodium beef jerky instead of chips and candy.
- Keep a small cooler with pre-portioned brown rice and beans from home, plus cut-up veggies.
For exercise, he started with 10-minute brisk walks around the parking lot while waiting on
deliveries, using a phone alarm as a reminder. Gradually, those walks became three 10-minute
sessions most days. Over several months, he noticed he could climb into his truck with less
effort and had fewer swelling episodes in his ankles.
Church Walking Club & Salsa Nights
In one predominantly Black and Hispanic neighborhood, a local church partnered with a nearby
clinic to start a heart-health program. After several members were hospitalized with heart
failure, the pastor decided that “faith without steps is dead” literally.
They started a Sunday-afternoon walking group, using the church parking lot and nearby
sidewalks. At first, it was mostly younger members, but older adults joined when they saw
that the pace was gentle and rest breaks were allowed. A few members with heart failure
walked with canes or used rollators. The rule was simple: move at your own pace, but move.
On Friday nights, the fellowship hall turned into a salsa and line-dancing space, with
low-sodium potluck dishes and water infused with citrus and mint. The laughter, music, and
sense of community made exercise feel more like celebration than “treatment.” People started
comparing pedometer steps, not just medications.
Learning to Speak Up at the Clinic
Many patients in these communities have had experiences where they felt rushed, ignored, or
stereotyped in health care settings. One middle-aged woman with heart failure shared that she
used to nod “yes” at every doctor’s appointment, then leave confused and scared.
With help from a community health worker, she wrote down three questions before each visit:
- “What’s my heart failure stage and what does it mean?”
- “What changes should I make to my food and activity this month?”
- “What should make me call you or go to the emergency room?”
Bringing that list and a family member changed the tone of her visits. Her doctor slowed
down, used simpler language, and referred her to cardiac rehab and a bilingual dietitian.
That support made it easier for her to stick with lower-sodium cooking and a walking plan,
and over time she felt more in control of her health.
Putting It All Together
Heart failure in Black and Hispanic communities is shaped by history, policy, and unequal
access not by any lack of willpower. But within those realities, diet and exercise are
powerful tools you can use every day to help your heart work better, reduce symptoms, and
protect your quality of life.
You don’t have to become a perfect eater or a marathon walker. You just have to make small,
steady changes that respect your culture and your circumstances: a little less sodium, a few
more vegetables, a few more minutes of walking, dancing, or chair exercises. Add in a care
team that listens and a community that supports you, and heart failure becomes something you
manage not something that always manages you.
SEO Summary & Metadata
with realistic tips tailored to culture, budget, and daily life.
sapo:
Heart failure affects Black and Hispanic communities earlier and more often but food and
movement can still shift the story. This in-depth guide explains how heart-healthy eating
and safe exercise ease symptoms, support medications, and fit into cultural traditions. From
lower-sodium twists on soul food and Latin favorites to realistic truck-stop strategies,
church walking clubs, and cardiac rehab, you’ll find practical, culturally grounded ideas to
protect your heart without giving up the flavors and routines you love.