Table of Contents >> Show >> Hide
- Peptic Ulcers 101: What’s Going On in There?
- Why Bananas Are Considered Ulcer-Friendly
- 16 Banana-Based Health Tips to Help Ease Peptic Ulcers
- 1. Choose the Right Ripeness
- 2. Start with Half a Banana at a Time
- 3. Pair Bananas with Soothing Carbs
- 4. Try a Mild Banana “Tummy Smoothie”
- 5. Combine Bananas with Probiotic-Rich Foods
- 6. Bake or Steam for Extra Gentleness
- 7. Keep Portions Moderate (Bananas Aren’t a Free-for-All)
- 8. Use Bananas as a Snack, Not a Late-Night Feast
- 9. Pair Bananas with Other Ulcer-Friendly Foods
- 10. Avoid “Banana Plus Trigger Food” Combos
- 11. Time Bananas Around Your Medications
- 12. Keep a Simple Food and Symptom Diary
- 13. Use Bananas as Part of Stress-Soothing Rituals
- 14. Don’t Ignore Red-Flag Symptoms
- 15. Consider Health Conditions That Affect Banana Intake
- 16. Remember: Bananas Support, Medicine Heals
- Other Lifestyle Steps That Work Well with Banana Therapy
- Practical “Real-Life” Experiences with Bananas and Peptic Ulcers
If your stomach feels like it’s auditioning for a volcano movie, you might be dealing with a peptic ulcer.
These small but mighty sores on the lining of your stomach or upper small intestine can cause burning pain,
nausea, and a serious fear of mealtimes. While medical treatment is absolutely essential, many people are
also curious about soothing, stomach-friendly foods – and bananas are at the top of that list.
So, can bananas actually help ease peptic ulcer symptoms? The short answer: they won’t cure ulcers, but they
can be a gentle, helpful part of an ulcer-friendly eating plan when used correctly. In this guide, we’ll walk
through what peptic ulcers are, why bananas are so often recommended, and 16 practical banana-based tips to
help calm your gut – plus other lifestyle strategies that matter just as much.
Important: Bananas (or any food) are not a replacement for proper medical care. If you suspect you have a peptic ulcer, you must see a healthcare professional for diagnosis and treatment.
Peptic Ulcers 101: What’s Going On in There?
A peptic ulcer is a sore in the lining of the stomach (gastric ulcer) or the first part of the small intestine,
the duodenum (duodenal ulcer). These sores develop when the protective lining of your digestive tract is damaged
and stomach acid or digestive enzymes have direct contact with the tissue underneath, causing irritation and pain.
Major causes include infection with Helicobacter pylori (H. pylori) bacteria and long-term use of
nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or aspirin. Smoking, heavy alcohol use, and chronic
stress can make things worse, but they’re usually not the primary cause by themselves.
Common symptoms include a burning or gnawing pain in the upper abdomen, discomfort that might improve or worsen
with eating, bloating, nausea, or feeling overly full. Some people have no noticeable symptoms at all until
complications appear, such as vomiting blood or passing black, tarry stools – which are medical emergencies.
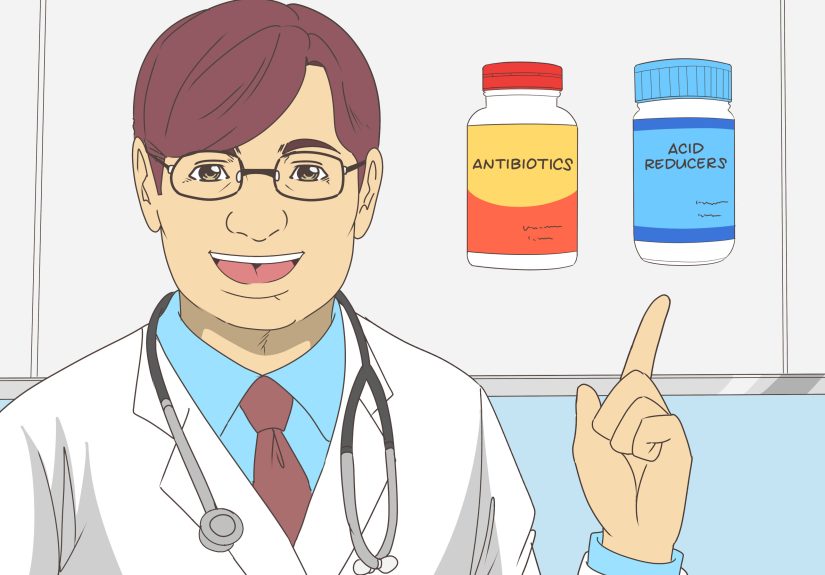
Standard treatment often includes medications like proton pump inhibitors (PPIs) or H2 blockers to reduce acid,
and antibiotics if H. pylori is present. Diet and lifestyle won’t replace these treatments, but they can support
healing and make day-to-day life more comfortable.
Why Bananas Are Considered Ulcer-Friendly
Bananas have been studied for their potential protective effects on the stomach lining, especially unripe or green
bananas and plantain-type bananas. Research suggests they may:
- Increase mucus production in the stomach, adding a protective layer over the lining.
- Provide compounds (like certain flavonoids and pectins) that may help protect against ulcer-causing agents in animal and lab studies.
- Offer gentle, low-acid, easily digestible carbohydrates and potassium, making them a friendly option when your stomach is sensitive.
That said, bananas are not miracle medicines. Human research is still limited, and experts are clear: bananas might
soothe and support, but they do not cure peptic ulcers or eradicate H. pylori. In fact, very ripe bananas
may increase acid production in some people. Think of bananas as a soft pillow for your stomach – comfy, but not a surgeon.
With that in mind, let’s get practical. Here are 16 banana-based tips to help you build an ulcer-friendly routine
that works with your treatment plan instead of trying to replace it.
16 Banana-Based Health Tips to Help Ease Peptic Ulcers
1. Choose the Right Ripeness
Green to yellow (but not overly speckled) bananas are usually the best starting point for people with peptic ulcers.
Slightly less ripe bananas tend to be less sugary and may contain more of the compounds that support mucus production
and protect the stomach lining. If you notice ripe bananas seem to increase your discomfort or acid, try dialing back
to slightly greener ones and see how your body responds.
2. Start with Half a Banana at a Time
When your stomach is already irritated, “gentle introduction” is the name of the game. Begin with half a banana per
snack rather than a whole one. Give yourself a couple of days to see how your symptoms react. If you feel comfortable,
you can slowly increase to one full banana at a time. If pain or burning worsens, talk with your healthcare provider
and cut back.
3. Pair Bananas with Soothing Carbs
Instead of eating bananas alone on an empty stomach, pair them with bland, ulcer-friendly carbohydrates like oatmeal,
rice porridge, or plain toast. A small bowl of oatmeal topped with sliced banana can offer soluble fiber plus a mild
sweetness, helping stabilize digestion and avoid sudden swings in stomach acid exposure.
4. Try a Mild Banana “Tummy Smoothie”
A simple banana smoothie can be easier to digest than a heavy meal. Blend:
- ½–1 banana
- A small amount of low-fat milk or a non-dairy alternative like oat milk
- A spoonful of plain yogurt (for probiotics, if tolerated)
Skip citrus juices, chocolate, and strong sweeteners. Keep it simple and mild so you aren’t accidentally triggering
more acid or reflux.
5. Combine Bananas with Probiotic-Rich Foods
Bananas contain prebiotic fibers that help nourish good gut bacteria. When paired with probiotic-rich foods like
yogurt or kefir (if you tolerate dairy), you’re giving your gut microbiome a supportive one-two punch. While probiotics
won’t cure ulcers either, a healthier gut environment may support long-term digestive comfort.
6. Bake or Steam for Extra Gentleness
If raw bananas feel heavy, try baking or lightly steaming them. Warm, soft banana can be easier on a sensitive stomach
and feels comfort-food cozy. Bake a peeled banana wrapped in parchment or foil until tender, then eat it plain or with
a small spoonful of plain yogurt.
7. Keep Portions Moderate (Bananas Aren’t a Free-for-All)
More bananas do not equal faster healing. Overeating in general can increase stomach pressure and worsen pain and reflux.
For most people with an otherwise balanced diet, 1–2 bananas spread across the day is plenty. Balance them with other
ulcer-friendly foods like lean proteins, cooked vegetables, and whole grains.
8. Use Bananas as a Snack, Not a Late-Night Feast
Eating right before bed can worsen reflux and nocturnal ulcer pain. If you’re going to reach for a banana, aim to do it
at least 2–3 hours before lying down. A small banana-and-oat snack in the afternoon or early evening is generally kinder
to your stomach than a midnight banana binge.
9. Pair Bananas with Other Ulcer-Friendly Foods
Bananas work best as part of an overall stomach-friendly way of eating. Build meals around:
- Lean proteins (like skinless poultry, tofu, or fish prepared without heavy frying)
- Cooked, non-acidic vegetables (such as carrots, squash, green beans, or potatoes)
- Whole grains and high-fiber foods that you tolerate well
Using bananas as a side or snack within this pattern supports your overall ulcer management plan.
10. Avoid “Banana Plus Trigger Food” Combos
A banana is gentle; a banana milkshake with chocolate syrup, strong coffee, and whipped cream is… less gentle.
Common ulcer and reflux triggers include alcohol, coffee, high-fat fried foods, chocolate, very spicy dishes, and
acidic foods like tomatoes and citrus. If you’re using bananas to calm your gut, don’t sabotage them by pairing them
with known irritants.
11. Time Bananas Around Your Medications
Many ulcer medications need to be taken on an empty stomach or a certain time before meals. Follow your prescriber’s
instructions carefully. In some cases, a small banana snack a bit later can help buffer acid and reduce discomfort
without interfering with how your medication works. If you’re unsure, ask your doctor or pharmacist whether bananas
are okay with your specific medicines.
12. Keep a Simple Food and Symptom Diary
Everyone’s stomach is a little different. While bananas are soothing for many, a few people may feel more bloated or
uncomfortable after eating them. Keeping a short daily diary – what you ate, when you ate it, and how your symptoms
felt – can help you and your healthcare provider fine-tune your diet. If bananas consistently help, you’ll see it.
If they don’t, you’ll catch that too.
13. Use Bananas as Part of Stress-Soothing Rituals
Stress doesn’t directly cause ulcers, but it can make symptoms worse and interfere with healing. Try turning
your banana snack into a mini self-care break: sit down, breathe slowly, chew thoroughly, and avoid scrolling through
your work emails while you eat. Calmer eating often means a calmer stomach.
14. Don’t Ignore Red-Flag Symptoms
If you have severe or persistent pain, unintentional weight loss, trouble swallowing, vomiting blood, or black, tarry
stools, this is not a “just eat a banana and see” situation. You need urgent medical evaluation. Bananas are not a shield
against serious complications like bleeding or perforation.
15. Consider Health Conditions That Affect Banana Intake
Bananas are high in potassium. For most people, that’s great. But if you have kidney disease or need to limit potassium
for other medical reasons, you’ll want to discuss safe serving sizes with your healthcare provider. People with diabetes
should also factor the natural sugar content of bananas into their carb management plan.
16. Remember: Bananas Support, Medicine Heals
The most important tip: view bananas as a supportive food, not a standalone ulcer cure. Peptic ulcers caused by H. pylori
infection usually require a combination of antibiotics and acid-suppressing medications. Ulcers related to NSAIDs often
need medication adjustments and protective therapies. Bananas can make you more comfortable along the way, but they cannot
replace proper diagnosis and treatment.
Other Lifestyle Steps That Work Well with Banana Therapy
To give your stomach the best chance at healing, combine banana-based tips with these proven strategies:
- Quit smoking if you smoke. Smoking impairs ulcer healing and increases recurrence risk.
- Avoid or limit alcohol, coffee, and highly spicy foods, which can aggravate pain in many people.
- Work with your doctor on NSAIDs – you may need to switch pain relievers or add protective medications.
- Eat smaller, more frequent meals rather than giant, heavy ones that overload your stomach.
- Maintain a balanced diet with plenty of fruits, vegetables, and fiber-rich foods you tolerate well.
- Manage stress with realistic tools like walking, gentle stretching, breathing exercises, or therapy.
When you put all these pieces together – medical care, smart food choices, stress management, and yes, the humble banana –
you create a much friendlier environment for your stomach to heal.
Practical “Real-Life” Experiences with Bananas and Peptic Ulcers
While everyone’s story is different, there are some recurring patterns in how people successfully use bananas as part of
their ulcer-care routine. Think of the following as composite “experiences” that combine what many patients report to
dietitians and gastroenterology teams.
One common pattern: the over-caffeinated office worker who lives on coffee and snacks and suddenly develops a burning pain
in the upper abdomen. After being diagnosed with a small duodenal ulcer, they’re prescribed medication and told to cut back
on coffee and late-night fast food. At first, the idea of eating anything in the morning feels scary. With guidance, they
start the day with half a banana and a small bowl of oatmeal instead of an oversized latte. Within a week or two, the intense
burning is less frequent. The key changer? Consistency: taking medication as prescribed, shifting to gentler foods, and using
bananas to bridge the gap between meals without overwhelming the stomach.
Another repeated story involves people who used to skip meals, then overeat. Long periods of an empty stomach can make ulcer
pain flare, and huge meals can flood the stomach with acid and stretch an already irritated lining. Many patients find that
a mid-morning and mid-afternoon banana-based snack – such as half a banana with a small yogurt, or banana slices over rice
cereal – helps prevent those major “I’m starving” crashes that lead to overeating. Their pain becomes more predictable and
often less intense simply because their eating pattern is steadier.
There are also people who learn, through trial and error, that not all banana situations are equal. One person might tolerate
raw bananas just fine but find that banana bread loaded with butter and sugar makes their ulcer flare. Another might love
thick banana smoothies but discover that when they’re made with chocolate or coffee, symptoms spike. What works for them
is stripping recipes back to basics: banana, mild milk or non-dairy alternative, maybe a bit of plain yogurt – and stopping
there. The simpler the recipe, the calmer their stomach.
Some people with ulcers also live with other conditions like diabetes, high blood pressure, or chronic kidney disease. Their
experience often involves balancing the potential benefits of bananas for their stomach with the need to manage blood sugar
or potassium levels. For example, instead of eating a whole banana at once, they might have a quarter or half banana paired
with a source of protein, such as a small portion of cottage cheese (if tolerated) or a spoonful of nut butter. This approach
keeps their blood sugar more stable while still providing that gentle, soothing texture on days when their ulcer is bothering
them.
Another recurring theme is emotional: people frequently feel anxious about eating when they have a peptic ulcer because
they associate food with pain. Working bananas into their routines can create a small sense of safety. A food that feels
familiar, soft, and non-threatening becomes a psychological ally as well as a physical one. Over time, as medications do
their job and symptoms improve, bananas may remain a go-to “comfort food” that reminds them they’re actively taking care
of their health.
It’s important to highlight that not every experience is positive. A few people find that bananas cause gas, bloating, or
discomfort. In those cases, forcing bananas because “they’re supposed to be good for ulcers” doesn’t make sense. The more
helpful pattern is personal experimentation guided by medical advice: try a small amount, notice how you feel, and adjust.
If bananas help, great – they have a place in your plan. If they don’t, there are plenty of other ulcer-friendly foods to
lean on instead.
Ultimately, the most successful stories with bananas and peptic ulcers share a common thread: bananas are one piece
of a bigger puzzle. People feel best when they combine banana-based snacks with regular follow-up visits, appropriate
medications, reduced use of ulcer-aggravating substances (like NSAIDs, alcohol, and tobacco), and a diet centered on
gentle, nutrient-dense foods. In that context, bananas aren’t magic – but they can be surprisingly comforting co-stars
in your healing journey.