Table of Contents >> Show >> Hide
- Quick Answer: Is Hummus Bad for Gout?
- Gout 101: Why Purines Matter
- Where Hummus and Chickpeas Land on the Purine Scale
- Plant-Based Purines vs. Animal Purines: Not All Purines Act the Same
- How Much Hummus Is Usually Okay for Gout?
- Other Purine-Rich Foods to Watch More Closely
- Building a Gout-Friendly Plate That Still Includes Hummus
- When You Might Want to Be More Careful with Hummus
- Practical Tips for Enjoying Hummus with Gout
- FAQs About Hummus, Purines, and Gout
- Real-Life Experiences: Navigating Hummus, Purines, and Gout
- Conclusion
If you love dipping warm pita into a big bowl of creamy hummus but also live with gout,
you’ve probably had this thought: “Is this little scoop of hummus going to make my toe
explode later?” The short answer: for most people with gout, hummus is not the villain.
But like most things in nutrition, the real answer is a little more nuanced.
In this article, we’ll break down how gout works, what purines are, where hummus lands on
the purine scale, and how to enjoy foods like chickpeas without sabotaging your joints.
We’ll also zoom out and look at other purine-rich foods, so you know what deserves your
attention more than a tablespoon of hummus.
Quick Answer: Is Hummus Bad for Gout?
For most people with gout or high uric acid:
- Hummus is generally considered a low-to-moderate purine food.
-
Chickpeas (the main ingredient in hummus) contain moderate levels of purines but don’t
appear to increase gout risk the way red meat and certain seafood do. -
A few spoonfuls of hummus as part of a balanced, mostly plant-based, gout-friendly diet is
usually fine for most people. -
The bigger gout culprits are organ meats, large portions of red meat, some seafood,
alcohol (especially beer), and sugary drinks.
Of course, everyone has different triggers. If you notice that hummus consistently lines up
with a flare, that’s important personal data even if it’s not on “official” high-purine lists.
Gout 101: Why Purines Matter
Gout is a type of inflammatory arthritis caused by the build-up of uric acid crystals in the
joints. Uric acid is the end product of purine breakdown purines being natural compounds
found in many foods and in your own cells.
Normally, uric acid dissolves in your blood and your kidneys filter it out in urine. If your
body makes too much uric acid or your kidneys can’t clear it efficiently, levels rise.
Eventually, needle-like crystals can form in joints (often the big toe first), causing:
- Sudden, intense joint pain
- Redness, warmth, and swelling
- Tenderness so severe even a bedsheet can hurt
That’s why doctors often recommend a lower-purine diet as one part of gout
management. You can’t avoid purines completely (you wouldn’t want to), but you can be strategic
about the types and sources you eat.
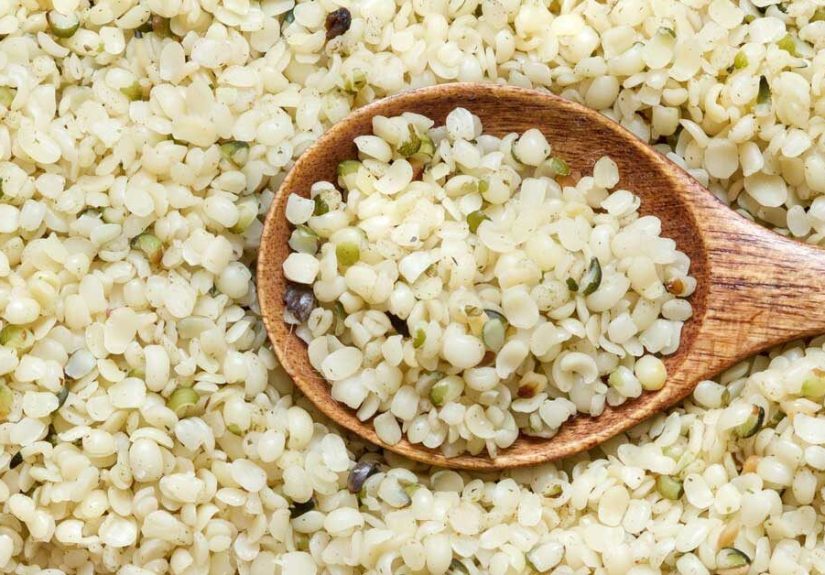
Where Hummus and Chickpeas Land on the Purine Scale
Let’s get more specific. Hummus is usually made from:
- Cooked chickpeas
- Tahini (ground sesame seeds)
- Olive oil
- Lemon juice
- Garlic and salt
The main source of purines here is chickpeas. Lab analyses suggest that dried
chickpeas (before cooking) typically fall into the moderate-purine range,
around 100–110 mg of purines per 100 grams of dry seed. Once soaked, cooked, and then turned
into hummus with tahini and other ingredients, the purine concentration per serving goes down
because you’re diluting the chickpeas and adding non-purine ingredients.
In most practical serving sizes:
- 2–4 tablespoons of hummus is a small to moderate purine load.
- Eating an entire tub in one sitting (we’ve all been there) is a bigger purine hit but still
not on the level of a steak or plate of organ meats.
Chickpeas vs. Classic High-Purine Foods
To put chickpeas and hummus in perspective, very high-purine foods often include:
- Organ meats (liver, kidney, sweetbreads)
- Certain fish and shellfish (anchovies, sardines, herring, mussels, scallops)
- Large portions of red meat
These can easily deliver 200 mg or more of purines per 100 g and are more
strongly linked to gout flares.
By comparison, chickpeas sit in the middle of the pack. They are:
- Higher in purines than, say, low-fat yogurt or most fruits
- Lower in purines than many meats and some seafood
- Packaged with fiber, plant protein, and beneficial nutrients
That last point matters more than you’d think.
Plant-Based Purines vs. Animal Purines: Not All Purines Act the Same
Here’s a twist that surprises a lot of people: research suggests that
purines from plant foods don’t seem to increase gout risk the same way that purines
from animal foods do.
Large studies looking at diet and gout risk have found:
-
Meat and certain seafood are strongly linked with higher gout risk and more
frequent flares. -
Plant-based proteins and vegetables, even when they contain purines (like
lentils, beans, peas, spinach, mushrooms), are much less strongly associated with gout
attacks. -
People eating more plant-based diets, Mediterranean-style diets, or DASH-style diets tend to
have a lower overall risk of gout.
Why the difference? Scientists think it’s partly because plant foods bring:
-
Fiber, which may help bind uric acid in the gut and support better blood
sugar and weight control. - Antioxidants and anti-inflammatory compounds, which help calm inflammation.
- Lower saturated fat, which supports metabolic and kidney health.
So while chickpeas and other legumes do contain purines, they’re also part of a bigger
nutrient package that appears protective, not harmful, in the long run for many
people with gout.
How Much Hummus Is Usually Okay for Gout?
There’s no single “official” hummus limit for gout, but we can make reasonable, gout-friendly
guidelines based on what we know about purines and plant-based diets.
For many people with gout, a sensible approach might look like:
-
Serving size: 2–4 tablespoons (about 30–60 g) of hummus at a time, not as
the entire meal but as part of a balanced plate. -
Frequency: A few times a week is usually fine, especially if the rest of
your diet is low in animal purines and sugary drinks. -
Balance: Pair hummus with plenty of low-purine foods like veggies and
whole-grain crackers instead of a large meat-heavy meal.
If your doctor or dietitian has given you a specific daily purine target (for example,
aiming for under a certain number of milligrams per day), you can think of hummus as a
moderate contributor that can fit into that budget, not something that
automatically breaks the bank.
Most importantly, track your own body’s response. If you eat hummus a couple of times a week
and feel fine, that’s a good sign. If you notice a pattern of flares after hummus-heavy meals,
it’s worth discussing with your healthcare provider and experimenting with smaller portions
or less frequent servings.
Other Purine-Rich Foods to Watch More Closely
If you’re going to stress about something, let it be the foods that are actually
strongly linked to gout flares in research, not your occasional snack of
hummus. Common higher-risk foods include:
1. Organ Meats and Certain Meats
- Liver, kidney, sweetbreads
- Large, frequent portions of beef, lamb, and pork
- Some processed meats and sausages
These are classic high-purine foods and are often recommended to be limited or avoided,
especially during gout flares.
2. Some Seafood
- Anchovies, sardines, herring, mackerel
- Mussels, scallops, and some shellfish
These can pack a heavy purine punch and may trigger flares in susceptible people.
3. Alcohol (Especially Beer) and Sugary Drinks
-
Beer and spirits can both increase uric acid and make it harder for your kidneys
to clear it out. -
Drinks sweetened with high-fructose corn syrup (sodas, some energy drinks) can also
raise uric acid levels.
Compared to these common triggers, hummus is a relatively low-stress choice especially if
you keep portions reasonable.
Building a Gout-Friendly Plate That Still Includes Hummus
The goal isn’t to have a sad, flavorless diet. It’s to build a
gout-friendly eating pattern that works for your joints, your labs, and
your taste buds.
A pattern similar to the Mediterranean or DASH diet often checks all of those boxes:
- Lots of vegetables and fruits
- Whole grains (brown rice, quinoa, oats, whole-grain bread)
- Plant-based proteins (beans, lentils, chickpeas, tofu, nuts, seeds)
- Moderate amounts of poultry and fish
- Low-fat or nonfat dairy
- Healthy fats like olive oil and avocado
Hummus fits right into this style of eating: it’s a plant-based protein spread
made with heart-healthy fats. Enjoy it with:
- Cucumber rounds, bell pepper strips, and carrot sticks
- Whole-grain crackers or pita
- A side of salad with olive oil and lemon dressing
This kind of meal gives you protein, fiber, and healthy fats all while keeping animal-based
purines in check.
When You Might Want to Be More Careful with Hummus
Even though hummus is generally safe, there are situations where you might want to be more
cautious:
-
During an acute flare: Some people choose to be extra conservative with all
purine-containing foods during a flare, focusing heavily on fruits, vegetables, low-fat
dairy, and fluids until the attack settles. -
If you’ve identified hummus as a personal trigger: Individual triggers
vary. If you notice a repeated pattern hummus today, gout flare tomorrow talk with your
doctor about it and consider temporarily reducing or eliminating it to see what happens. -
If you have kidney disease or very high uric acid: Your healthcare team may
want to fine-tune all sources of purines more carefully, including plant-based ones.
Remember: this article is for general education and is not a replacement for
medical advice. Always follow the guidance of your doctor or registered dietitian, especially
if you’re on uric acid–lowering medications or have other health conditions.
Practical Tips for Enjoying Hummus with Gout
-
Watch the portion, not just the food. A few tablespoons of hummus are very
different from eating an entire container in one sitting. -
Pair hummus with low-purine dippers. Fresh veggies or whole-grain crackers are
better choices than stacking it on a meat-heavy sandwich. -
Check the ingredient list on store-bought hummus. Some brands add lots of oil,
salt, or sugar. These don’t change purine content but can affect weight, blood pressure, and
overall inflammation. -
Make your own hummus. You can use less salt, more lemon, extra garlic, or blend
in roasted veggies (like red peppers or carrots) for more nutrients and flavor. -
Think about the whole day. If you’re planning hummus at lunch, maybe keep dinner
lighter on animal protein and skip that extra beer or sugary soda. -
Stay hydrated. Drinking enough fluids helps your kidneys flush out uric acid more
effectively.
FAQs About Hummus, Purines, and Gout
Is hummus considered a high-purine food?
No. Hummus is made from chickpeas, which are a moderate-purine legume. Because hummus
also contains tahini, olive oil, and other ingredients, the overall purine concentration per serving is
typically moderate. It’s nowhere near organ meats or certain seafood in terms of purine density.
Can I eat hummus every day if I have gout?
It depends on your total diet, portion sizes, and personal triggers. Many people with gout can enjoy a
small serving of hummus daily as part of a low-meat, plant-forward eating pattern. If you’re unsure,
start with a few times a week, track how you feel, and discuss your pattern with your doctor or dietitian.
Are other bean dips safe for gout?
Most bean-based dips (black bean dip, lentil spreads, white bean hummus) contain moderate purines but
also offer fiber and plant protein. In reasonable portions, they’re generally preferable to meat-heavy
dishes. Again, watch for personal triggers, portion sizes, and what else you’re eating and drinking.
What’s more important: avoiding hummus or cutting back on alcohol and red meat?
If we’re ranking priorities, cutting back on alcohol, sugary drinks, organ meats, and large
amounts of red meat is far more impactful than worrying about a side of hummus with veggies.
Real-Life Experiences: Navigating Hummus, Purines, and Gout
Because food choices are so personal, it can help to think through how different people might approach
hummus and purine-rich foods in real life. These examples are fictional but based on common patterns
seen in people living with gout.
Mark: The Meat-and-Beer Guy Who Blamed the Hummus
Mark is in his 40s, loves weekend barbecues, and recently had his first gout flare. The attack hit after
a party where he had burgers, wings, several beers, and for good measure half a tub of hummus with
chips. At his doctor’s visit, Mark was convinced hummus was the problem because it was the “healthy”
thing he remembered eating.
After reviewing his habits, his doctor and dietitian gently pointed out that the beer, red meat,
and overall portion sizes were much more likely culprits. Instead of banning hummus, they worked
on:
- Limiting beer and switching to more non-alcoholic options
- Cutting back on red meat and adding more poultry and plant-based meals
- Keeping hummus to a few tablespoons with veggie sticks, not an entire bag of chips
A few months later, Mark still enjoys hummus regularly but as part of a much more gout-friendly meal
pattern and his flares have become much less frequent.
Linda: The Plant-Based Eater Who Still Gets Flares
Linda has eaten mostly plant-based for years but still has gout flares. She rarely drinks alcohol and
doesn’t eat meat, so she wondered if her chickpeas, lentils, and hummus were to blame. Her healthcare
team ran a full workup and found that while her purine intake was moderate, she also had kidney
function issues and a strong family history of gout.
In Linda’s case, the solution wasn’t to cut out all legumes (which are central to her diet) but to:
- Fine-tune portions of certain high-purine plant foods
- Increase low-fat dairy, fruits, and vegetables further
- Start medication to control uric acid more aggressively
She found she could still enjoy hummus several times a week as long as her overall diet stayed balanced
and her medication kept uric acid in target range.
Sam: The Data Tracker
Sam is a numbers person who tracks everything in an app steps, water intake, and yes, gout flares. When
he started logging his food carefully along with symptoms, a pattern emerged: his flares lined up with
heavy meat meals and nights of beer or sugary soda, not with days where he had hummus and veggie
snacks.
With that information, Sam decided to:
- Use hummus as his go-to protein snack at work
- Swap at least two meat-heavy dinners each week for plant-based meals
- Cut his soda habit and increase water intake
Over time, his flares became less frequent and less intense. The data reassured him that hummus could be
part of the solution, not the problem.
What These Stories Tell Us
These examples illustrate a few key points:
-
Context matters. A small serving of hummus in an otherwise balanced diet is very different
from a hummus-plus-meat-plus-beer feast. -
Individual triggers vary. Your gout pattern is unique; tracking your own flares and food
choices can reveal surprising insights. -
Plant foods are rarely the sole villains. For many people with gout, the bigger wins come
from cutting back on animal purines, alcohol, and sugary drinks rather than micromanaging a modest serving
of hummus.
At the end of the day, the question isn’t just “Is hummus bad for gout?” It’s “How does hummus fit into my
overall lifestyle, lab values, and personal symptom patterns?” For most people, the good news is that this
creamy, flavorful dip can stay on the menu in moderation while you and your healthcare team focus on the
bigger levers that truly move the needle for gout.
Conclusion
Hummus and chickpeas are not top-tier enemies in a gout-friendly diet. They sit in the
moderate-purine category, but research suggests that plant-based purines don’t carry the same risk as those
from red meat, organ meats, and certain seafood. When eaten in reasonable portions and paired with a mostly
plant-forward, low–sugar, lower–alcohol lifestyle, hummus can be a delicious, satisfying, and joint-friendly
part of your menu.
Work with your healthcare team, pay attention to your body’s patterns, and remember: it’s usually the
overall pattern of what you eat and drink not one specific food like hummus that makes
the biggest difference for gout.