Table of Contents >> Show >> Hide
- Quick refresher: What PCOS actually is (and isn’t)
- Menopause basics: the timeline everyone deserves in plain English
- So what’s the connection? PCOS doesn’t “end”it evolves
- Does PCOS change the age you reach menopause?
- Symptoms that overlap (and confuse everyone): PCOS vs. perimenopause
- Health risks to pay extra attention to after 40 if you have PCOS
- Management: What to do in perimenopause and after menopause if you have PCOS
- A midlife “PCOS + menopause” checkup checklist
- When to seek care sooner (not later)
- The bottom line: the “connection” is your long-term health trajectory
- Experiences from real life: What people with PCOS often notice during perimenopause and beyond (about )
If you have PCOS, you’ve probably already learned an annoying truth: hormones rarely “wrap things up neatly.”
Menopause can feel like it should be a grand finalecurtain closed, cycles done, end of story. But PCOS doesn’t
exactly take a bow and leave the stage. Instead, it changes costumes.
The real connection between polycystic ovary syndrome (PCOS) and menopause is this: PCOS is not just about periods
or fertility. It’s a lifelong metabolic-and-hormonal condition that can keep influencing your health long after your
last menstrual cycle. The good news? Once you understand what shifts (and what doesn’t), you can plan smarter for
the decades ahead.
Quick refresher: What PCOS actually is (and isn’t)
PCOS is a common hormone-related condition. Despite the name, the “cysts” aren’t the main issueand not everyone
with PCOS has them. PCOS is usually diagnosed based on a combination of:
- Ovulatory dysfunction (irregular or absent ovulation, often seen as irregular periods)
- Hyperandrogenism (higher “androgen” activitythink acne, unwanted hair growth, scalp hair thinning)
- Polycystic-appearing ovaries on ultrasound (sometimes, not always)
Many people with PCOS also deal with insulin resistance, weight changes, and higher risk for conditions like
prediabetes and type 2 diabetes. So while PCOS often shows up in the reproductive years, its “long game” is more
about metabolic health than monthly calendars.
Menopause basics: the timeline everyone deserves in plain English
Menopause is officially defined as 12 consecutive months without a period (assuming there’s no other cause).
The years leading up to it are called perimenopausethe transition when hormone levels fluctuate and periods can
become unpredictable.
In the U.S., the average age for menopause is roughly around 51–52, but “normal” can still be a wide range.
Common menopause-transition symptoms include hot flashes, night sweats, sleep disruption, mood changes, vaginal dryness,
and shifts in body composition.
So what’s the connection? PCOS doesn’t “end”it evolves
Here’s the heart of it: menopause ends ovulation and periods, but it doesn’t automatically erase the hormonal and metabolic
patterns linked to PCOS. Some PCOS features may soften with age, while others stick around (or become more noticeable
when estrogen drops).
1) Period problems may disappear… but that doesn’t mean PCOS did
If irregular cycles were your loudest PCOS symptom, menopause can feel like a strange kind of reliefno more guessing
whether your period is “late” or simply ghosting you again. But the disappearance of periods is a menopause milestone,
not a PCOS cure. The underlying tendenciesespecially insulin resistance and cardiometabolic riskcan persist.
2) Androgens often decline with age, but “relative androgen excess” can persist
Testosterone and other androgens generally trend downward with age, including after menopause. However, research suggests
that people with PCOS may still show higher androgen activity compared to peers even in peri- and postmenopause.
Translation: you may still notice unwanted hair growth, acne flares, or scalp hair thinningthough patterns can change.
3) Metabolic risk is the biggest overlapand it matters more in midlife
Menopause itself is associated with changes that can worsen cardiometabolic risk: increases in visceral (abdominal) fat,
worsening cholesterol patterns, and rising blood pressure risk. If PCOS already put you closer to that edge, the menopause
transition can feel like the risk dials turn faster.
That doesn’t mean disaster is inevitable. It does mean the “connection” between PCOS and menopause is less about ovaries
and more about what’s happening in your metabolism, blood vessels, liver, and pancreas over time.
Does PCOS change the age you reach menopause?
You’ll see mixed messaging on thisbecause the evidence is mixed. Some studies report that people with PCOS may reach
menopause slightly later than those without PCOS, while other analyses find little to no difference overall.
Differences in study design, how PCOS was diagnosed, body weight, smoking, and genetics can all influence results.
The practical takeaway: don’t assume you’ll have an early menopause because you have PCOS. If anything, some evidence
points the opposite direction. But the more important issue is not the exact birthday of menopauseit’s managing
long-term risk factors along the way.
Symptoms that overlap (and confuse everyone): PCOS vs. perimenopause
PCOS and perimenopause can share several symptoms, which is why midlife can feel like a detective novel written by
your endocrine system:
- Irregular cycles: classic in PCOS, also common in perimenopause
- Weight changes: can occur in both, especially around the abdomen
- Mood shifts: anxiety, irritability, low moodcommon in both (and in life, frankly)
- Sleep issues: can be driven by hot flashes, stress, sleep apnea risk, or all of the above
One clue is the type of symptoms: hot flashes and night sweats are more characteristic of the menopause transition.
Another clue is your history: PCOS typically starts earlier in life, even if it wasn’t diagnosed until later.
Health risks to pay extra attention to after 40 if you have PCOS
Prediabetes and type 2 diabetes
PCOS is strongly linked to insulin resistance, which raises the risk of prediabetes and type 2 diabetes.
Importantly, diabetes risk can be elevated even in people with PCOS who are not in larger bodies.
Midlife is a smart time to get serious about screening and prevention.
Example: A 44-year-old with “lean PCOS” may feel dismissed because her BMI is normal, but she can still have insulin
resistance and rising A1C. Catching that early can prevent years of silent progression.
Cholesterol, blood pressure, and metabolic syndrome
PCOS is associated with unfavorable lipid patterns and higher rates of metabolic syndrome. The menopause transition can
further shift cholesterol and blood pressure in an unfavorable direction. Think of it as a “two-factor authentication”
system for risk: PCOS plus menopause transition may increase the need for consistent monitoring.
Heart and vascular health
People with PCOS often have more cardiovascular risk factors, but research is still evolving on whether that translates
into clearly higher rates of cardiovascular events later in life for all groups. Meanwhile, menopause itself is a known
turning point for cardiovascular risk in many women.
The sensible plan: treat cardiovascular prevention as a priorityoptimize blood pressure, lipids, glucose, sleep, activity,
and stress managementrather than waiting for a “perfect” risk prediction.
Sleep apnea
Obstructive sleep apnea is more common in PCOS and can worsen insulin resistance, blood pressure, and fatigue. If you snore loudly,
wake up gasping, have morning headaches, or feel unrefreshed despite enough sleep, it’s worth discussing evaluation.
Endometrial health and postmenopausal bleeding
In the reproductive years, long stretches without ovulation can expose the uterine lining to “unopposed estrogen,” raising the risk of
endometrial hyperplasia and endometrial cancer over time. After menopause, any vaginal bleeding should be evaluated promptly,
regardless of PCOS history.
Example: If a 58-year-old who had PCOS gets spotting months or years after her final period, she shouldn’t chalk it up to
“hormones being weird.” It’s a medical check-in moment.
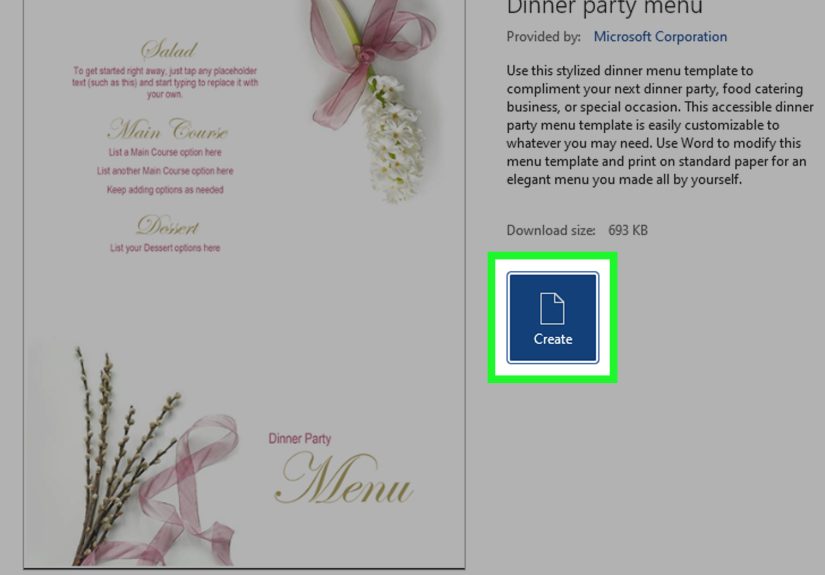
Management: What to do in perimenopause and after menopause if you have PCOS
PCOS management in midlife is less about ovulation calendars and more about protecting long-term health. A practical plan often includes
a mix of lifestyle strategies, targeted screening, and (when needed) medications.
Lifestyle: boring advice that works (with a better sales pitch)
- Strength training: improves insulin sensitivity and supports bone and muscle as estrogen declines
- Fiber-forward eating: helps glucose control, cholesterol, and satiety (your gut will write you thank-you notes)
- Protein distribution: supports muscle maintenance and appetite regulation
- Sleep consistency: not glamorous, but a powerful metabolic lever
- Stress management: cortisol doesn’t cause PCOS, but chronic stress can worsen sleep, cravings, and blood sugar
Medical options to discuss with your clinician
Your best choices depend on symptoms, age, risk factors, and whether you still need contraception. Options may include:
- Metformin for insulin resistance or prediabetes risk (common in PCOS care)
- Anti-androgen approaches (for acne or hirsutism), when appropriate and monitored
- Targeted cholesterol or blood pressure treatment if lifestyle changes aren’t enough
- Menopause symptom treatment (including hormone therapy for some people), based on individual risk/benefit
If you’re considering hormone therapy for menopause symptoms, it’s especially important to discuss your overall cardiometabolic profile,
whether you have a uterus (which affects whether progesterone/progestin is needed with estrogen), and your personal and family history.
A midlife “PCOS + menopause” checkup checklist
Bring this list to your next appointment and watch your clinician quietly admire your organization (even if they don’t say it out loud):
- Glucose screening: A1C and/or oral glucose testing as recommended based on your risk profile
- Lipids: total cholesterol, LDL, HDL, triglycerides
- Blood pressure: both in-office and home readings if needed
- Weight and waist circumference: trends matter more than one number
- Sleep screening: especially if snoring, daytime sleepiness, or resistant hypertension
- Mental health check: anxiety/depression screening and support options
- Bleeding review: any abnormal bleeding patterns (and any postmenopausal bleeding should be evaluated)
When to seek care sooner (not later)
- New or heavy bleeding, bleeding after sex, or any bleeding after menopause
- Symptoms of high blood sugar (excess thirst/urination, blurry vision, unusual fatigue)
- Chest pain, shortness of breath, or new exercise intolerance
- Severe sleep disruption, loud snoring, or waking up gasping
- Rapid hair loss, new severe acne, or signs of high androgens that change suddenly
The bottom line: the “connection” is your long-term health trajectory
PCOS and menopause connect in the way two weather systems connect: one (PCOS) sets the baseline climate, and the other (menopause transition)
brings a new front of hormonal change. You can’t control every forecast, but you can absolutely prepareespecially by focusing on metabolic
health, cardiovascular prevention, sleep, and prompt evaluation of abnormal bleeding.
And if you take nothing else from this: menopause doesn’t erase PCOS, but it also doesn’t doom you. With the right monitoring and a
few strategic habits, midlife can be less “hormonal chaos” and more “informed adulting.”
Experiences from real life: What people with PCOS often notice during perimenopause and beyond (about )
Everyone’s experience is unique, but clinicians and patient communities often describe a few common patterns when PCOS and menopause overlap.
Below are composite, real-world-style scenarios (not a substitute for medical advicethink of them as “you’re not alone” snapshots).
“My periods were always irregular… so how will I even know I’m in perimenopause?”
This is one of the most common frustrations. If your cycles have been unpredictable since your teens or twenties, the classic early sign of
perimenopause (cycle changes) can feel unhelpful. Many people report that vasomotor symptomshot flashes, night sweats, and a sudden
intolerance for warm roomsbecome the clearer clue. Others notice a new kind of sleep disruption: waking at 3 a.m. with a brain that wants to
reorganize the entire pantry.
“My acne came back like it pays rent.”
Some people with PCOS say their skin improves as they age; others report flare-ups during perimenopause. Even though overall hormone levels are
declining, the fluctuations can make skin feel unpredictable. People often describe experimenting again with topical treatments, simplifying
skincare, or revisiting medications they used years ago. A frequent emotional theme is annoyance: “I thought I was done with this after 25.”
“The scale changed, but the bigger issue was where the weight went.”
Many report that weight gain in their forties and fifties isn’t just about poundsit’s about abdominal fat distribution and feeling like their
body composition changed even when routines stayed similar. People often describe needing to shift from mostly cardio to adding strength training,
increasing protein, and paying closer attention to sleep. Some also report that stress and caregiving responsibilities make consistent routines harder,
which is a real (and underappreciated) factor in metabolic health.
“My labs were ‘fine’… until they weren’t.”
A common story is that someone with PCOS had borderline glucose or cholesterol numbers for years, then saw a noticeable shift during the menopause
transition. This is where people often say they became more proactivetracking blood pressure at home, requesting repeat labs, or working with a
clinician to set earlier prevention goals. Many describe feeling empowered once they moved from “waiting to see what happens” to “let’s not let it happen.”
“Hair changes got emotionally loud.”
Unwanted facial hair can persist, and scalp hair thinning can become more noticeable in midlife. People frequently describe the “maintenance” part
as exhaustingtweezing, waxing, laser, changing hairstyles, trying supplements, or comparing before/after photos in bathroom lighting that feels personally
insulting. The most helpful experience reports often involve a combination approach: realistic expectations, medical evaluation when changes are sudden,
and practical cosmetic strategies that reduce daily stress.
If these experiences sound familiar, the main message isn’t “this is your destiny.” It’s that many people with PCOS benefit from treating midlife as a
strategic health phaseone where prevention, symptom support, and clear screening plans make a measurable difference.