Table of Contents >> Show >> Hide
- First: A 60-Second Map of SMA Treatment Options
- Questions to Ask About Diagnosis, Genetics, and “What Type of SMA Is This?”
- Questions to Ask About Disease-Modifying Treatments (Spinraza, Evrysdi, Gene Therapies)
- Questions to Ask About Combination Therapy, Switching, or “What If This Isn’t the Right Fit?”
- Questions to Ask About Supportive Therapies (Because Medication Isn’t the Whole Story)
- Questions to Ask About Monitoring Progress (So You’re Not Guessing)
- Questions to Ask About Access, Insurance, and the Not-So-Fun Paperwork Side of Medicine
- Questions to Ask About Clinical Trials and What’s Coming Next
- Questions to Ask at Different Life Stages
- Conclusion: Bring the Right Questions, Not the Perfect Answers
- Real-World Experiences: What the SMA Journey Often Looks Like (and What People Wish They’d Asked Earlier)
Getting a spinal muscular atrophy (SMA) diagnosis can feel like someone handed you a 300-page instruction manual… for a device you didn’t buy… in a language you don’t speak… and the “Help” button is missing. The good news: SMA care has changed dramatically in the last several years, and there are now disease-modifying treatments plus a deep bench of supportive therapies that can protect strength, breathing, swallowing, and daily function.
The tricky part is that “SMA treatment” isn’t one single decision. It’s a long-term strategy built around your (or your child’s) age, SMA type, symptoms, genetics, goals, lifestyle, and tolerance for tradeoffsbecause every option has them. This guide is a practical list of smart, specific questions to ask your neuromuscular team so you can walk into appointments feeling prepared, not surprised.
First: A 60-Second Map of SMA Treatment Options
Most treatment plans combine two big categories:
- Disease-modifying treatments (DMTs): therapies designed to increase survival motor neuron (SMN) protein or replace the missing/defective SMN1 functionaiming to slow progression and improve outcomes.
- Supportive therapies: respiratory care, nutrition/swallow support, physical and occupational therapy, mobility equipment, orthopedic care, and morebecause muscles don’t live in isolation, no matter how much they try to.
In real life, most people with SMA benefit from a coordinated, multidisciplinary care teamneurology plus pulmonary/respiratory, PT/OT, nutrition, speech/swallow, orthopedics, rehab medicine, and social work. It’s not “extra”; it’s the strategy.
Questions to Ask About Diagnosis, Genetics, and “What Type of SMA Is This?”
Before you can choose a therapy, you need clarity on what you’re treating. SMA can vary widely, and early details shape the entire plan.
Ask about the genetics behind the diagnosis
- “Which genetic test confirmed SMA, and what exactly did it show?”
- “Do we know the SMN2 copy number, and how does that influence expected severity and urgency?”
- “Is this 5q SMA (SMN1-related), or something that mimics SMA?”
- “Should our family meet with a genetic counselor, and should relatives consider carrier testing?”
Ask what “type” meansand what it doesn’t
- “Based on symptoms and milestones, which SMA type best fits right now?”
- “How often does the label change as kids grow (or as treatments change the trajectory)?”
- “What are the most realistic goals for the next 6 months, 12 months, and 2 years?”
Pro tip: you’re not being “difficult” by asking for specifics. You’re being efficient. SMA care works best when decisions are shared and goals are explicit.
Questions to Ask About Disease-Modifying Treatments (Spinraza, Evrysdi, Gene Therapies)
Disease-modifying SMA therapies differ in how they’re given, who is eligible, what monitoring is needed, and what the day-to-day burden looks like. The best choice is the one that matches medical needs and real-life logistics.
Big-picture decision questions (start here)
- “Which SMA treatment options are medically appropriate for us right nowand why?”
- “How does age, weight, current function, scoliosis/spine anatomy, or respiratory status affect eligibility?”
- “What outcomes are most likely: gaining skills, stabilizing, slowing decline, improving endurance?”
- “How quickly do you expect to see changes, and how will we measure them?”
- “If we don’t see improvement, how do we decide whether the treatment is still working?”
Questions to ask about Spinraza (nusinersen)
Spinraza is an intrathecal therapy (delivered into spinal fluid) with a loading schedule and ongoing maintenance doses.
- “How is the procedure done for our situationstandard lumbar puncture, imaging-guided, sedation?”
- “What does the schedule look like for loading doses and long-term dosing?”
- “What labs or monitoring do you do before each dose (platelets, coagulation, urine protein, etc.)?”
- “What are the common side effects you see in your clinic, and what should trigger a call?”
- “If spinal anatomy makes access difficult (scoliosis, spinal fusion), what are our options?”
- “What does ‘success’ look like for infants vs teens vs adults on Spinraza?”
Questions to ask about Evrysdi (risdiplam)
Evrysdi is taken orally once daily and dosing depends on age and body weight. It can be appealing because it’s non-invasivethough “daily forever” is its own kind of commitment.
- “What dose applies to us, and how is it adjusted over time (growth, weight changes)?”
- “Should it be taken with food, and what happens if a dose is missed?”
- “If swallowing is difficult, can it be given through a feeding tubeand how?”
- “What side effects should we watch for, and what labs or follow-up do you recommend?”
- “Are there pregnancy, fertility, or contraception considerations we should discuss (especially for teens/adults)?”
- “How do you track whether daily oral therapy is workingfunction tests, fatigue, respiratory metrics?”
Questions to ask about gene therapy options (Zolgensma, and newer FDA-approved gene therapy for age 2+)
Zolgensma is a one-time intravenous gene therapy approved for children under 2 years of age. Newer FDA-approved gene therapy has expanded treatment to patients age 2 and older via intrathecal administration (into spinal fluid). Gene therapy can be powerfulbut it comes with specific safety monitoring and timing considerations.
- “Are we eligible for gene therapy based on age, weight, and overall health?”
- “What pre-treatment testing is required (including liver function, platelets)?”
- “Will steroids be needed before/after, and what’s the plan for monitoring labs afterward?”
- “What are the most important safety risks you worry about, and how do we reduce them?”
- “How do vaccines and recent infections affect timing?”
- “If we choose gene therapy, what supportive therapies should start immediately to maximize gains?”
- “Can someone receive another SMA DMT later, and what evidence or clinic experience guides that decision?”
Questions to Ask About Combination Therapy, Switching, or “What If This Isn’t the Right Fit?”
Families often want a simple “best treatment” answer. In reality, SMA treatment planning looks more like: best option for this body, at this time, with these constraints.
- “Do you ever use sequential or combination approaches in your practice? In which scenarios?”
- “What would make you recommend switching therapiesfunction changes, side effects, access issues?”
- “How long do you typically monitor before deciding whether a therapy is benefiting someone?”
- “If treatment is stopped, what’s the plan to watch for changes and restart if needed?”
Practical note: if your appointment feels like speed dating with pharmacology, ask for a follow-up visit focused only on decision-making. It’s a lot to process in one sitting.
Questions to Ask About Supportive Therapies (Because Medication Isn’t the Whole Story)
Disease-modifying therapy is foundational, but supportive care is where day-to-day function is protectedand where quality of life can improve in very tangible ways.
Physical therapy and occupational therapy
- “What PT/OT goals make the most sense for our current strength and endurance?”
- “How do we build strength safely without overfatiguing (especially with SMA-related weakness)?”
- “What home exercises actually matterand which ones are mostly busywork?”
- “What adaptive equipment could help now (standing devices, orthotics, seating, hand supports)?”
Respiratory care
- “What’s our baseline respiratory status, and how often should it be monitored?”
- “Do we need cough-assist, suction, noninvasive ventilation, or sleep studies?”
- “What’s our ‘sick-day plan’ for colds and respiratory infections?”
- “Which warning signs mean we should go to urgent care or the ER?”
Swallowing, nutrition, and GI support
- “Should we get a swallow evaluation, and what would it change?”
- “How do we prevent aspiration and support safe feeding?”
- “What nutrition goals support strength and energy without causing reflux or fatigue?”
- “When should we consider feeding support (like a G-tube), and what are the pros/cons?”
Orthopedics, mobility, and posture
- “How are we monitoring scoliosis, hip stability, and contractures?”
- “What seating or positioning changes could reduce pain and improve breathing?”
- “When do braces helpand when do they just make life harder?”
- “What mobility options (wheelchair, power assist, walkers) fit our goals right now?”
Questions to Ask About Monitoring Progress (So You’re Not Guessing)
“Feels better” is importantbut in SMA, objective tracking matters because changes can be subtle, slow, or masked by normal growth and development. Your clinic may use standardized motor scales, respiratory measures, and functional assessments.
- “Which tests or scales do you use (and are they appropriate for age and SMA type)?”
- “How often will we measure motor function, breathing, and swallowing?”
- “What counts as meaningful improvementnew skills, longer endurance, fewer hospitalizations?”
- “Are there ‘red flags’ that suggest we need to adjust the plan sooner?”
- “Can we track fatigue and daily function, not just clinic-day performance?”
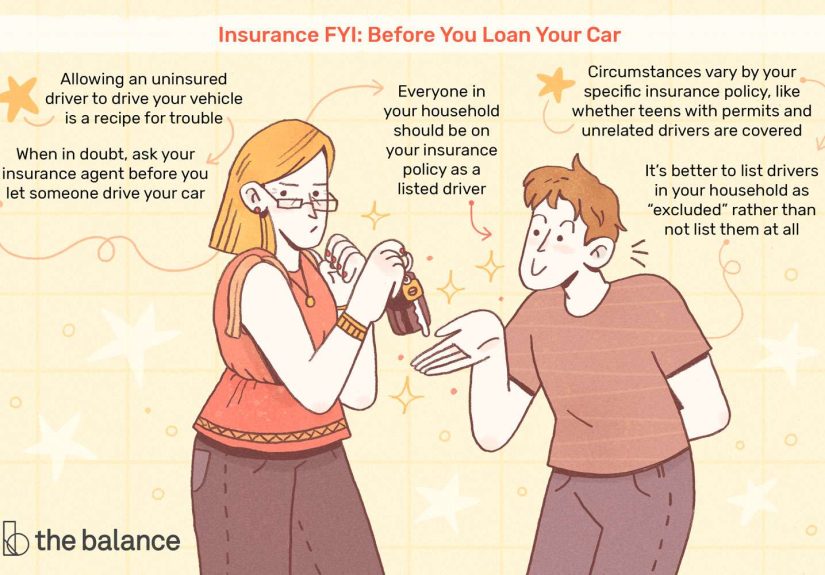
Questions to Ask About Access, Insurance, and the Not-So-Fun Paperwork Side of Medicine
SMA therapies can be expensive and access can be complicated. The paperwork is not a moral test of your worthiness. It’s just paperwork that happens to have teeth.
- “Which prior authorizations are needed, and who submits them?”
- “What documentation does insurance usually require (genetic confirmation, functional scores, history)?”
- “If we’re denied, what’s the appeal planand how quickly can we act?”
- “Are there manufacturer support programs or foundations that can help with copays or travel?”
- “If treatment requires travel to a specialty center, can care be shared locally for labs or therapies?”
Questions to Ask About Clinical Trials and What’s Coming Next
SMA research is active, and many families want to know what’s in the pipelineespecially if current therapies don’t fully meet goals.
- “Are there clinical trials appropriate for our age and SMA type right now?”
- “If we join a trial, how does it affect access to approved treatments?”
- “What is the study measuringmotor milestones, endurance, biomarkers, quality of life?”
- “What are the time commitments and risks, and what happens after the trial ends?”
If your clinic doesn’t run trials, ask where they refer patients and how to evaluate opportunities safely. “New” is exciting, but “well-designed” is the real glow-up.
Questions to Ask at Different Life Stages
For newborns and infants (including after newborn screening)
- “How quickly do we need to start treatment, and what steps happen first?”
- “What immediate supportive care helps right nowfeeding, breathing, positioning?”
- “What milestones are realistic, and how do we support development without overwhelm?”
For school-age kids
- “How do we coordinate therapies with school and fatigue management?”
- “What accommodations should be in place (IEP/504, mobility, bathroom access, emergency plans)?”
- “How do we support independence without turning the house into an obstacle course?”
For teens and adults
- “How do we balance treatment benefits with time, energy, and daily responsibilities?”
- “What pain, fatigue, or mental health supports are recommended?”
- “Are there reproductive health considerations we should plan for?”
- “How do we handle transition from pediatric to adult care (or between systems)?”
Conclusion: Bring the Right Questions, Not the Perfect Answers
SMA treatment and therapies are no longer just about “managing decline.” For many people, the goal is improved function, preserved independence, and fewer complicationssupported by disease-modifying therapies and a coordinated care team. The most powerful tool you bring to the clinic isn’t medical jargon. It’s clarity: what matters to you, what tradeoffs you can live with, and what success should look like in your real life.
If you want a simple next step, try this: pick 10 questions from this article, paste them into your phone notes, and bring them to your next visit. Your future self will thank youand your appointment will feel less like a pop quiz you didn’t study for.
Real-World Experiences: What the SMA Journey Often Looks Like (and What People Wish They’d Asked Earlier)
The clinic version of SMA treatment is tidy: prescribe therapy, schedule follow-ups, measure progress, repeat. The real-life version is messierbecause it includes school schedules, work meetings, insurance portals that time out for sport, and a child (or adult) who is understandably not thrilled about being “a medical project.”
One of the most common experiences families describe is the emotional whiplash of progress that comes in tiny, meaningful pieces. It might not be a dramatic “first steps” moment. Sometimes it’s: fewer choking episodes at dinner, a stronger cough during a cold, or a kid who can sit longer without getting exhausted. Those wins count. They’re also easy to miss if you’re only looking for headline moments. Many families find it helpful to keep a simple “function journal” for a few minutes a weekwhat got easier, what got harder, what changed with fatigue. It turns vague impressions into useful data for the care team.
Another shared reality: treatment days can be a whole event. For intrathecal dosing, it may involve travel, imaging guidance, sedation planning, and recovery timeplus the emotional load of a procedure day. People often say the best improvement they made was building a “procedure-day routine” that includes comfort items, favorite shows, snacks (for after), and a plan for the rest of the day that is intentionally light. Not lazystrategic. The body is doing work.
With daily oral therapy, the challenge can be consistency. Families talk about how easy it is to start strong and then slowly drift when life gets chaotic. Helpful hacks often include: setting a daily phone alarm, linking dosing to a reliable routine (like brushing teeth), and keeping a backup plan for travel days. A surprisingly frequent lesson: don’t wait until you’re out to refill. Medication logistics have their own calendar and they do not care about your vacation.
Insurance and access issues are, unfortunately, part of the SMA landscape. Many caregivers describe learningagainst their willhow to speak fluent Prior Authorization. The families who feel least powerless aren’t the ones who never get denied; they’re the ones who build a system: a binder (or digital folder) with genetic test results, clinic notes, functional assessments, denial letters, appeal templates, and names/extensions of the people they spoke with. It’s not fun. It’s also weirdly empowering to have receipts.
Finally, many people say the best “therapy” decision they made was not a medication choiceit was embracing multidisciplinary care early. PT/OT, respiratory support, swallow evaluations, mobility equipment, and seating/positioning changes can make daily life dramatically safer and easier. The turning point often comes when someone realizes that using equipment is not “giving in.” It’s gaining capacity. A power chair doesn’t steal independence; it returns it. A cough-assist isn’t pessimism; it’s preparedness.
If there’s one emotional thread that shows up again and again, it’s this: SMA families become experts, but they shouldn’t have to become exhausted. Asking clear questions, getting plans in writing, and insisting on follow-up when something doesn’t make sense isn’t being “a lot.” It’s being the steady voice in a system that can be loud and confusing. And yessometimes humor helps. If you can laugh at the absurdity of a 14-page fax about a one-page approval, take the laugh. You earned it.