Table of Contents >> Show >> Hide
- What is septic arthritis?
- What septic arthritis looks like (a “picture” guide)
- Septic arthritis symptoms you shouldn’t ignore
- What causes septic arthritis?
- How septic arthritis is diagnosed
- Treatment options for septic arthritis
- Can septic arthritis be prevented?
- Living through septic arthritis: real-world–style experiences
- Conclusion
When most people think of “joint problems,” they picture slow, creaky arthritis that shows up over years.
Septic arthritis is not that. It’s the “drop everything and go to the hospital” version of joint trouble
a true medical emergency where an infection attacks a joint and can destroy cartilage in a matter of days.
In this guide, we’ll walk through what septic arthritis is, what it typically looks like in real-life and
medical pictures, key symptoms you should never ignore, and the treatment options doctors use to protect
your joint and your life. We’ll also share some real-world–style experiences to help you understand what
it actually feels like to go through septic arthritis and recover from it.
What is septic arthritis?
Septic arthritis (also called infectious arthritis) is a joint infection. Bacteria, a virus,
or a fungus gets into the joint space usually the knee, hip, shoulder, or ankle and causes intense
inflammation of the synovial fluid and the joint lining. That swelling and inflammation quickly damage
cartilage and bone if not treated right away.
It’s considered an orthopedic emergency. Without rapid antibiotics and joint drainage, septic
arthritis can lead to permanent joint damage, chronic pain, disability, and even life-threatening sepsis.
Septic arthritis can affect:
- Adults of any age, but especially older adults and people with other health conditions.
- Children and babies, where it can show up as fussiness, refusing to walk, or not using a limb.
- People with joint replacements, where a prosthetic joint can also become infected.
What septic arthritis looks like (a “picture” guide)
If you search “septic arthritis pictures,” the clinical photos and imaging can look dramatic and honestly,
a little scary. Here’s what those pictures usually show and how that translates to real life.
Common visual signs in real life
-
Red, hot joint: The skin over the joint looks flushed or red compared with surrounding skin.
If you put your hand over it, it often feels noticeably warmer than the other side. -
Obvious swelling: The joint may look puffy or ballooned, with lost normal shape for example,
a knee that looks like a tight, shiny ball instead of its usual contours. - Severe tenderness: Even light touch or gentle movement can cause sharp pain.
-
Limited motion: In pictures, you’ll often see the joint held in a “comfort” position slightly
bent because straightening or bending it more hurts too much.
What medical imaging pictures show
Doctors often use imaging alongside physical exam and lab tests. Typical images might include:
-
Ultrasound images: These pictures show excess joint fluid (an effusion) and help guide a needle
into the joint to draw out fluid for testing. -
X-ray pictures: Early on, X-rays might look almost normal, but over time they can show joint space
narrowing, bone damage, or dislocation if the infection is severe or delayed. - MRI images: These show inflammation, bone involvement (osteomyelitis), and soft tissue changes around the joint.
While pictures are helpful, they are not a substitute for urgent evaluation. If you or someone you love has
a suddenly hot, swollen, painful joint especially with fever do not wait to “see what it looks like tomorrow.”
Go to an emergency department or urgent care right away.
Septic arthritis symptoms you shouldn’t ignore
Core symptoms in adults
Septic arthritis symptoms typically come on quickly over hours to a couple of days. Common signs include:
- Severe joint pain that worsens with movement and is often present even at rest.
- Swelling and a feeling of tightness or fullness in the joint.
- Warmth and redness over the joint.
- Very limited range of motion you may not be able to walk, put weight on the joint, or move it without intense pain.
- Fever and chills (though not everyone will have a fever, especially older adults or people with weakened immune systems).
- Feeling generally very sick, tired, or “off,” sometimes with nausea or rapid heartbeat if sepsis develops.
Symptoms in babies and children
Kids don’t always say, “My knee is red and swollen and I think I have a joint infection.” Instead, you might see:
- Refusing to walk, crawl, or use an arm or leg.
- Holding a limb in one position and crying when it’s moved.
- Fever, irritability, or poor feeding in infants.
- Swelling and warmth around a joint (often the hip, knee, or ankle).
When to call 911 or go to the ER
Seek emergency care right away if:
- You have a sudden, severe, hot, swollen joint plus fever or chills.
- You feel very unwell or confused, or your heart is racing.
- The pain is so intense you can’t move the joint, walk, or bear weight.
- You recently had an injection, surgery, or injury to that joint and symptoms are rapidly worsening.
Septic arthritis gets harder not easier to treat the longer it goes undiagnosed. Early treatment can mean
the difference between a full recovery and lasting damage or disability.
What causes septic arthritis?
The most common cause of septic arthritis is bacteria that enter the joint and multiply. The usual suspects include:
- Staphylococcus aureus (including MRSA) the top cause in adults.
- Streptococcus species especially in people with skin infections or bloodstream infections.
- Neisseria gonorrhoeae a sexually transmitted infection that can cause gonococcal septic arthritis, especially in younger adults.
- Other bacteria, including those from animal bites or injuries (for example, scratches, pecks, or bites that puncture the joint area).
- Less commonly, fungi, mycobacteria (like tuberculosis), or viruses.
The germs usually reach the joint in one of three ways:
- Through the bloodstream from another infection site (skin, lungs, urinary tract, etc.).
-
Directly into the joint from a puncture wound, surgery, injection, or penetrating injury
(including animal-related injuries). - From nearby tissue if an infection in bone or soft tissue spreads into the joint.
Risk factors for septic arthritis
Although septic arthritis can occur in otherwise healthy people, your risk is higher if you have:
- Older age (especially over 65–80).
- Diabetes, kidney disease, liver disease, or lung disease.
- Rheumatoid arthritis or other inflammatory joint diseases.
- A joint replacement (hip, knee, shoulder prosthesis).
- Recent joint surgery or injection into a joint.
- Skin infections, chronic ulcers, or open wounds.
- Conditions or medications that weaken your immune system (for example, cancer treatments, steroids, biologic drugs, HIV).
- Injection drug use or heavy alcohol use.
How septic arthritis is diagnosed
Doctors diagnose septic arthritis by combining your symptoms, physical exam, lab tests, and imaging. The key
test is almost always a joint fluid analysis.
Step 1: History and physical exam
Your healthcare provider will ask about:
- When the pain and swelling started, and how quickly it worsened.
- Whether you’ve had recent infections, injuries, bites, surgeries, or injections.
- Your medical conditions, medications, and any history of joint problems.
They’ll examine the joint for warmth, redness, swelling, and limited range of motion, and they’ll check for
signs of systemic infection such as fever, low blood pressure, or rapid heart rate.
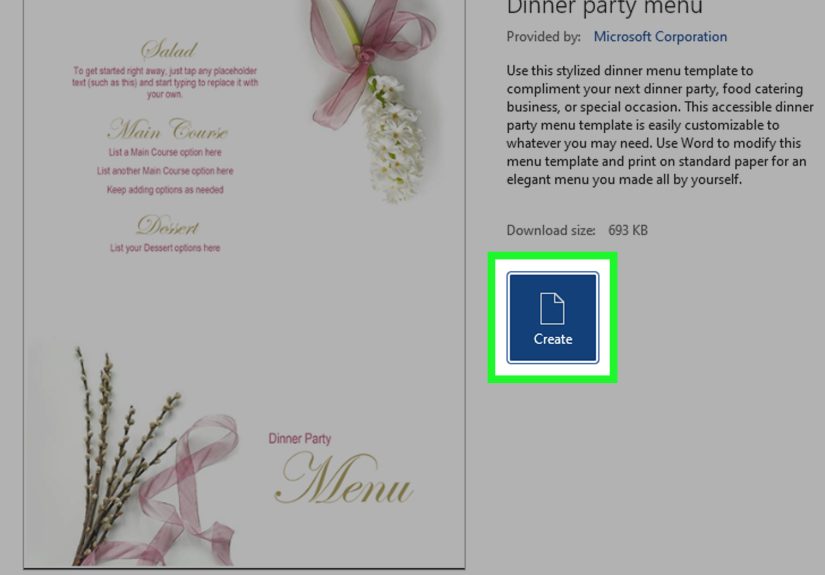
Step 2: Joint aspiration (arthrocentesis)
This is the gold-standard test. The clinician:
- Cleans the skin and inserts a sterile needle into the joint space.
- Draws out synovial fluid often cloudy, thick, or purulent (“pus-like”) in septic arthritis.
- Sends the fluid to the lab to check cell counts, crystals, Gram stain, and cultures.
High white blood cell counts and positive cultures strongly support the diagnosis. Arthrocentesis also
helps relieve pressure and pain by removing excess fluid.
Step 3: Blood tests and imaging
Additional tests may include:
- Blood cultures to see if infection is in the bloodstream.
- Inflammatory markers (ESR, CRP), which are usually elevated.
- X-rays, ultrasound, or MRI to look at joint damage, effusion, and nearby bone.
Treatment options for septic arthritis
Septic arthritis treatment has two main goals: clear the infection and protect the joint.
That usually requires a combination of antibiotics and joint drainage, often in the hospital.
1. Rapid antibiotics
Once doctors suspect septic arthritis, they typically start intravenous (IV) antibiotics right away
often before culture results are final to cover the most likely bacteria. Later, they adjust the medication
once lab results identify the specific organism and its antibiotic sensitivities.
Common points about antibiotic treatment:
- Initial treatment is usually IV for several days.
- If you’re improving and stable, you may switch to oral antibiotics.
- Total treatment time is often 2 to 4 weeks for many cases, and sometimes longer for more complicated infections, resistant bacteria, or prosthetic joints.
Taking antibiotics exactly as prescribed and not stopping early just because you feel better is crucial to
fully clear the joint infection.
2. Joint drainage and surgery
Infection thrives in closed spaces. That’s why drainage is just as important as antibiotics. Depending
on the joint and how severe the infection is, your team may use:
- Repeated needle aspiration: Using a needle to drain fluid from the joint once or multiple times.
-
Arthroscopic washout: A minimally invasive surgery in which small instruments and a camera are
inserted into the joint to flush out infected fluid and debris. - Open surgery: Used for large joints, difficult-to-drain joints (like the hip), or severe infections.
The choice depends on factors such as which joint is affected, how fast the infection progressed, your overall
health, and whether you have a prosthetic joint.
3. Pain control, splinting, and physical therapy
While the infection is being treated, the joint may be:
- Immobilized with a splint initially to control pain.
- Treated with medications for pain and fever (as appropriate for your health history).
Once the infection is improving, physical therapy usually begins to:
- Restore range of motion.
- Rebuild strength.
- Reduce stiffness and help you return to daily activities.
4. Possible complications and long-term outlook
Even with good care, septic arthritis can sometimes cause:
- Permanent joint damage or cartilage loss.
- Chronic pain and reduced mobility.
- Osteomyelitis (bone infection) or spread of infection elsewhere.
- Sepsis and increased mortality risk, especially if treatment is delayed or if you have serious underlying conditions.
The good news: when septic arthritis is caught early and aggressively treated, many people recover with good
or near-normal joint function.
Can septic arthritis be prevented?
Not every case can be prevented, but you can lower your risk with some practical steps:
- Clean cuts, puncture wounds, and animal bites promptly and seek medical care when recommended.
- Follow post-surgery and post–joint injection instructions closely.
- Manage chronic conditions like diabetes, kidney disease, and autoimmune diseases as advised by your provider.
- Get prompt treatment for skin infections, urinary tract infections, and other bacterial infections.
- Talk with your healthcare team if you have a joint replacement and notice new pain, swelling, or warmth in that joint.
Living through septic arthritis: real-world–style experiences
Reading about joint fluid analysis and antibiotic regimens is one thing. Living through septic arthritis is
another. While everyone’s story is different, many patients describe similar emotional and physical milestones.
The “something is really wrong” moment
For many, the story starts with what feels like a minor issue a sore knee after a hike, a small cut near the
ankle, or a flare of what they assume is regular arthritis. Then, usually overnight, the pain ramps up far
beyond anything they’ve experienced before.
Imagine this: you go to bed thinking, “My knee’s a bit sore.” By morning, it’s twice the size, red, hot, and
you can’t put your foot on the floor without a lightning-bolt stab of pain. Even the weight of a bedsheet feels
like too much. That’s often the point where people realize this isn’t a typical ache.
Hospital, tests, and tough decisions
In the emergency department, things move fast: blood pressure cuff, temperature, IV line, blood draws, and
then the big one joint aspiration. For many patients, the idea of a needle into the joint is nerve-wracking,
but they’re usually surprised by the relief that follows once some of the fluid is drained.
When the fluid looks cloudy or purulent and labs show very high white blood cell counts, the diagnosis shifts
from “maybe gout or a flare” to “this is likely septic arthritis.” At that moment, the care team usually
starts IV antibiotics and calls orthopedic or rheumatology specialists to plan drainage or surgery.
Recovery is a marathon, not a sprint
After surgery or repeated aspirations, pain often improves noticeably within a few days, but recovery doesn’t
end when you leave the hospital. Patients commonly describe:
- Fatigue: Fighting infection plus antibiotic side effects can leave you wiped out for weeks.
-
Fear of re-injury: People are often nervous about putting weight on the joint or stretching it
“too far,” which makes working with a physical therapist especially important. -
Frustration with limitations: Everyday tasks like climbing stairs, driving, or kneeling can feel
like obstacle courses during those first months.
Over time, with consistent rehab, many patients regain strong function. Some return to walking long distances,
playing with grandkids on the floor, or getting back to hobbies that once felt out of reach. Others may have
some lasting stiffness or occasional pain, especially after a long day a reminder of what their joint went through.
Emotional impact and mindset shifts
Septic arthritis doesn’t just attack joints; it also shakes your sense of security in your body. Many people
report:
- Heightened awareness of fevers, infections, and new joint pain.
- More respect for “small” injuries a tiny puncture wound or animal scratch no longer feels trivial.
- Gratitude for mobility: Walking without pain, driving, or bending down becomes something they actively appreciate, not just expect.
On the positive side, going through septic arthritis often turns people into their own best advocates. They
learn to speak up when something feels wrong, to ask questions about tests and treatment options, and to push
for timely care when symptoms don’t make sense.
What to remember if you’re worried about septic arthritis
If you’re reading this because you’re worried you or someone you love might have septic arthritis, here are
three key takeaways:
- Do not wait it out. A hot, swollen, very painful joint is not something to monitor at home for a few days.
- Emergency care is appropriate. You are not “overreacting” by going to the ER this is exactly what emergency departments are for.
- Early treatment changes outcomes. Rapid antibiotics and drainage can protect your joint and dramatically improve long-term function.
Always consult a healthcare professional or seek emergency care if you suspect septic arthritis. Online
information including this article is for education, not for diagnosis or treatment decisions.
Conclusion
Septic arthritis is a serious, fast-moving joint infection that requires equally fast action. The typical
“picture” a red, hot, swollen, extremely painful joint, often paired with fever or feeling very sick
should trigger urgent medical evaluation, not a wait-and-see approach.
Understanding what septic arthritis looks like, recognizing the symptoms, and knowing the standard treatment
options (antibiotics, drainage, surgery when needed, and rehab) helps you act quickly if it ever appears in
your life or your family’s. With early, aggressive care, many people avoid long-term complications and get
back to the activities that matter most to them.