Table of Contents >> Show >> Hide
- Why Your Body Does This (Yes, It’s Dramatic on Purpose)
- Common Causes of Vomiting and Diarrhea at the Same Time
- Quick Clue Guide: What Your Symptoms Might Suggest
- Management: What to Do First (and What to Skip)
- When to Seek Medical Care (Don’t “Wait It Out” in These Cases)
- What a Clinician May Do (So It’s Less Mysterious)
- Prevention: How to Avoid a Repeat Episode
- FAQ: Quick Answers to Common Questions
- Real-World Experiences (500+ Words): What People Commonly Go Through
- Conclusion: The Smart Game Plan
- SEO Tags
Not a fun club to join, but extremely common. When vomiting and diarrhea hit together, it can feel like your digestive system staged a coordinated walkout: the stomach is rejecting everything northbound while the intestines are fast-tracking everything southbound. The good news? In many healthy people, this “coming out both ends” episode is short-lived and treatable at home with smart hydration, rest, and a little strategy. The important news? Sometimes it’s a warning sign of dehydration or an infection that needs medical careespecially in kids, older adults, pregnant people, and anyone with a weakened immune system.
This guide breaks down the most common causes, what symptoms mean (and what they don’t), how to manage it safely, and exactly when it’s time to stop Googling and call a healthcare professional.
Why Your Body Does This (Yes, It’s Dramatic on Purpose)
Vomiting and diarrhea are defense mechanisms. If your body thinks you swallowed something harmfullike a virus, bacteria, or toxinit may try to eject it quickly. That can mean nausea and vomiting to clear the stomach, plus diarrhea to flush the intestines. Unfortunately, this “emergency evacuation plan” can also sweep out a lot of water and electrolytes (sodium, potassium, etc.), which is why dehydration is the main risk.
Common Causes of Vomiting and Diarrhea at the Same Time
1) Viral gastroenteritis (aka “stomach flu,” though it’s not influenza)
This is the #1 culprit in many cases. Viruses like norovirus and rotavirus can inflame the lining of your stomach and intestines, causing sudden nausea, vomiting, watery diarrhea, cramps, and sometimes fever or body aches. Norovirus is especially contagious and often spreads through close contact, contaminated food, or shared surfaces.
- Typical timing: Symptoms often start suddenly and improve within 1–3 days for many people.
- Common clue: Someone around you (family, classmates, coworkers) had the same symptoms recently.
2) Food poisoning
Foodborne illness can be caused by viruses (like norovirus), bacteria (like Salmonella, Campylobacter, Shigella, certain E. coli), parasites, or toxins produced in contaminated food. Your symptoms depend on the germ and how much you ate.
- Fast onset (1–6 hours): Often suggests a toxin (for example, improperly stored foods). Vomiting can be intense.
- Later onset (6 hours to several days): More typical of bacterial infections.
- Red-flag clue: Bloody diarrhea, severe abdominal pain, or high fever can signal an invasive infection that needs medical evaluation.
Example: You ate undercooked poultry at a cookout and 1–3 days later develop fever, cramping, diarrhea, and vomitingthis pattern fits several common foodborne bacteria and deserves extra caution, especially if symptoms are severe.
3) “Traveler’s diarrhea”
Travelespecially to regions with different food and water sanitation standardscan expose you to bacteria or parasites that your gut isn’t prepared for. Symptoms may include watery diarrhea, cramps, and sometimes vomiting.
4) Medications, supplements, and alcohol irritation
Some antibiotics, NSAIDs (like ibuprofen), iron supplements, magnesium-containing products, and certain other medications can irritate the GI tract or disrupt gut bacteria, causing nausea, vomiting, and diarrhea. Heavy alcohol intake can also inflame the stomach lining.
5) Anxiety, motion sickness, and migraine-triggered nausea (with a GI twist)
Stress and anxiety can increase gut motility and trigger nausea. Migraines can cause vomiting and stomach upset. These usually don’t cause significant watery diarrhea on their own, but they can make a viral or dietary issue feel worseand sometimes symptoms overlap.
6) Less common (but important) causes
Most “both ends” episodes are infections, but some situations need urgent evaluation, such as severe dehydration, appendicitis-like abdominal pain, bowel obstruction, pancreatitis, or metabolic problems. If you have severe pain, confusion, fainting, or blood in stool or vomit, don’t try to tough it out.
Quick Clue Guide: What Your Symptoms Might Suggest
These clues are not a diagnosisjust pattern recognition to help you decide how cautious to be.
| Pattern | Often Seen With | What to Do |
|---|---|---|
| Sudden vomiting + watery diarrhea; others sick too | Viral gastroenteritis (often norovirus) | Hydrate, rest, prevent spread; watch for dehydration |
| Vomiting starts within hours after a meal | Food toxin-type food poisoning | Hydrate; seek care if severe or persistent |
| Fever and/or bloody diarrhea | Invasive bacterial infection | Medical evaluation recommended; avoid anti-diarrheals |
| Symptoms last >48 hours with no improvement (adults) | Ongoing infection, dehydration risk | Consider calling a clinician |
| Young child/infant with vomiting + diarrhea | Higher dehydration risk | Call pediatrician early; use oral rehydration solution |
Management: What to Do First (and What to Skip)
Step 1: Hydration is the main treatment
Your top priority is replacing fluid and electrolytes. Plain water helps, but when vomiting and diarrhea are both happening, electrolyte loss matters.
- Best option: Oral rehydration solutions (ORS) sold over the counter (often marketed for kids, but useful for adults too). They’re designed to absorb well even when your stomach is cranky.
- If you’re vomiting: Take small, frequent sipsthink 1–2 mouthfuls every few minutes. Big gulps can trigger more vomiting.
- Helpful “micro” strategies: Ice chips, tiny sips, or a spoonful every few minutes can be easier than drinking a full glass.
Dehydration signs to watch for: intense thirst, dry mouth, dizziness, dark urine or peeing less, unusual sleepiness, and in children, fewer wet diapers and no tears when crying.
Step 2: Foodgo gentle, but don’t starve the gut
Old-school advice sometimes pushes ultra-restricted diets for days. Current guidance is more practical: once you can keep fluids down and your appetite returns, eat as tolerated. A restricted diet doesn’t speed recovery for viral gastroenteritis in most cases.
Try these “low-drama” foods first:
- Toast, crackers, rice, oatmeal
- Bananas, applesauce
- Soup/broth (also helps with sodium)
- Plain noodles or potatoes
- Small portions more often (your stomach appreciates low expectations)
Hold off (temporarily) if they worsen symptoms: greasy foods, very spicy foods, alcohol, and large amounts of sugary drinks (some people find they worsen diarrhea).
Step 3: Medicationsuse thoughtfully (and sometimes not at all)
Over-the-counter options can be helpful in specific situations, but they’re not “automatic.”
- Anti-diarrheals (like loperamide/Imodium): These may help some adults with watery diarrhea, but they should be avoided if you have fever, bloody diarrhea, or suspicion of invasive infection. They’re also generally not recommended for children and teens unless a clinician specifically advises it.
- Bismuth subsalicylate (Pepto-Bismol): Can reduce diarrhea in some adults. It contains a salicylate, so it’s not appropriate for everyone (including people allergic to aspirin). It also has important warnings for children and teenagers recovering from viral illnesses due to the risk of Reye’s syndromeso don’t give it to kids/teens unless a clinician says it’s okay.
- Anti-nausea medicines: If vomiting prevents you from keeping any fluids down, a clinician may prescribe an antiemetic (for example, ondansetron in certain cases) to help you tolerate oral rehydration.
- Antibiotics: Not useful for viral gastroenteritis and can sometimes make diarrhea worse. They’re only used when a clinician suspects or confirms certain bacterial or parasitic infections.
Important: If you’re unsure about medicationsespecially for kids, teens, pregnancy, older adults, or chronic medical conditionscall a healthcare professional. The “right” choice depends on symptoms and risk factors.
Step 4: Rest and recovery (yes, your body needs the nap)
Illness plus dehydration can make you feel wiped out. Rest helps your immune system do its job. If you can sleep, do it. If you can’t, at least lie down and stop negotiating with your stomach.
Step 5: Prevent spreading it to everyone you like
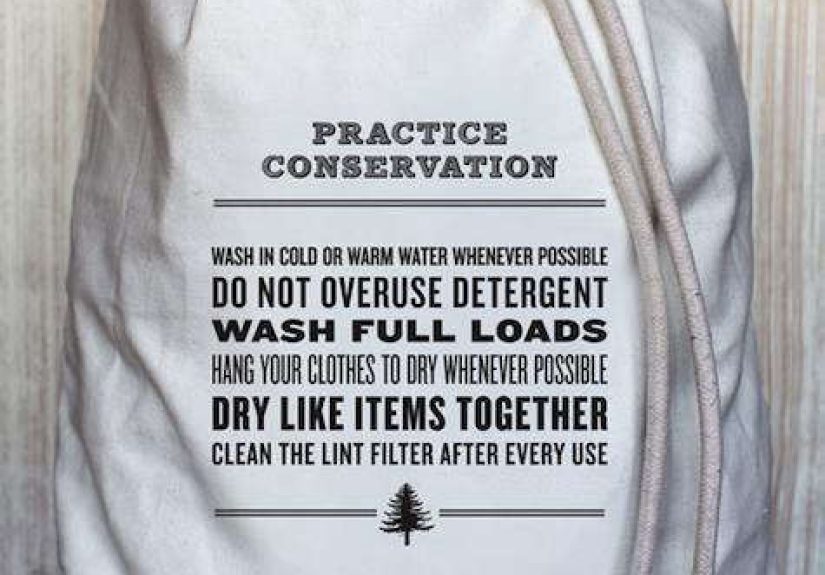
If a virus like norovirus is the cause, it spreads easily. Basic hygiene makes a big difference:
- Wash hands with soap and water (especially after bathroom trips and before eating or preparing food).
- Clean and disinfect contaminated surfaces. Follow product labels; household bleach-based disinfection is commonly recommended for norovirus cleanup. Never mix bleach with ammonia or other cleaners, and ventilate the area.
- Avoid preparing food for others while sick and for at least 48 hours after symptoms stop.
- Wash soiled laundry promptly and dry thoroughly.
When to Seek Medical Care (Don’t “Wait It Out” in These Cases)
Call a healthcare professional or seek urgent care if any of the following apply:
For adults
- You can’t keep fluids down for many hours, or you’re getting more dehydrated.
- Diarrhea lasts more than 2 days without improvement.
- You have severe abdominal or rectal pain.
- You have a high fever (for example, 102°F or higher).
- Your stool contains blood or pus, or stools are black and tarry.
- You feel faint, confused, unusually sleepy, or have signs of severe dehydration.
For infants and children
- Any signs of dehydration (fewer wet diapers, no tears, unusual sleepiness, dry mouth).
- Vomiting often or diarrhea lasting more than a day.
- Any fever in infants, or high fever in older children.
- Blood in stool, severe belly pain, or a child who seems significantly less responsive than usual.
Higher-risk groups who should call earlier
- Older adults
- Pregnant people
- People with immune suppression or significant chronic conditions (kidney disease, heart disease, diabetes, etc.)
What a Clinician May Do (So It’s Less Mysterious)
If you seek care, the goal is usually to prevent complications and treat any specific cause that needs it.
- Check hydration: Vital signs, exam findings, sometimes blood or urine tests.
- Replace fluids: Oral rehydration when possible; IV fluids if you’re severely dehydrated or can’t keep anything down.
- Testing: Stool tests if you have blood, high fever, severe symptoms, recent travel, or an outbreak concern.
- Targeted treatment: Anti-nausea medication, and antibiotics only when appropriate.
Prevention: How to Avoid a Repeat Episode
- Handwashing: Soap and water beats wishful thinking.
- Food safety basics: Clean, separate, cook, and chill. Avoid risky foods (undercooked meats/eggs, unpasteurized products, unwashed produce).
- Vaccination: Rotavirus vaccine (for infants) reduces severe gastroenteritis risk.
- Smart travel habits: Be cautious with water sources and high-risk foods in unfamiliar settings.
FAQ: Quick Answers to Common Questions
Is it okay to drink sports drinks?
Sometimes. They can help with mild fluid loss for adults, but oral rehydration solutions are designed to replace electrolytes more effectivelyespecially for kids or significant diarrhea.
Should I “stop eating” until it passes?
Not usually. Focus on fluids first. Once you can keep fluids down and you’re hungry, return to gentle foods and then your regular diet as tolerated.
How do I know if it’s food poisoning or a stomach virus?
It can be hard to tell. A very fast onset after eating can suggest a toxin; multiple people sick after the same meal points toward foodborne illness; outbreaks in schools, households, and cruise settings often point to viruses. Regardless, hydration and red-flag screening matter most.
Real-World Experiences (500+ Words): What People Commonly Go Through
When people describe vomiting and diarrhea at the same time, the emotional theme is surprisingly consistent: “I was not prepared.” Even people who’ve had stomach bugs before often underestimate how quickly dehydration can sneak up when both symptoms hit together.
Experience #1: The “I tried to be tough” adult. A common story goes like this: someone gets a sudden wave of nausea at night, vomits, then realizes diarrhea has joined the party. They decide to sleep it offonly to wake up dizzy, with a dry mouth and a headache. What tends to help most in these accounts isn’t a miracle pill; it’s a small behavioral change: taking tiny sips of an electrolyte drink every few minutes instead of waiting until they’re “ready” to drink. People often say the first hour of sipping is miserable, but after that, they can keep fluids down more reliably and the nausea calms.
Experience #2: The “kiddo contagion boomerang.” In families, the pattern is often: one child brings home a stomach virus, and within days, multiple people are negotiating for bathroom time like it’s a shared resource. Parents commonly report two things that made a real difference: (1) having oral rehydration solution on hand before anyone gets sick, and (2) switching from “drink a whole cup” to “one teaspoon or one sip every couple of minutes” when vomiting won’t stop. Many also mention calling the pediatrician sooner than they expected, especially when a child is less playful, urinates less, or can’t keep fluids down. That early call often prevents a middle-of-the-night urgent care trip.
Experience #3: The “restaurant roulette” situation. People who suspect food poisoning often point to a meal that seemed fine at the timebuffet food that sat out, undercooked meat, or a creamy dish on a hot day. Their symptoms may start with intense nausea and repeated vomiting, followed by diarrhea and cramping. In these stories, what helps is a “minimum expectations” plan: rest, small sips, simple foods, and being cautious with anti-diarrheals if fever or blood shows up. People frequently say they felt better when they stopped forcing heavy meals and instead focused on fluids, broth, and bland foods until appetite returned naturally.
Experience #4: The “I cleaned… and still got sick” frustration. With highly contagious viruses like norovirus, people often feel annoyed that they “did everything right” and still got ill. A practical lesson from many real-life outbreaks is that handwashing and surface disinfection reduce risk but don’t make it zeroespecially in close quarters. People also mention that the “second wave” of illness in a household often comes from shared bathrooms, doorknobs, phones, and towels. The tactic that shows up repeatedly: assigning separate towels, cleaning high-touch areas, and avoiding food prep for others until at least two days after symptoms stop.
Experience #5: The recovery hangover. Even after vomiting stops, many people report lingering fatigue or a “delicate stomach” for a few days. They often do best with smaller meals and gradually reintroducing normal foods. Some notice temporary sensitivity to rich or greasy foods, which is basically your gut saying, “Let’s not sprint on a sprained ankle.” The consistent takeaway: hydration first, then gentle food, then normal lifeat a pace your body can tolerate.
Conclusion: The Smart Game Plan
Vomiting and diarrhea at the same time is usually your body reacting to an infection or toxinand most cases improve with supportive care. Your best tools are surprisingly unglamorous: oral rehydration (small, steady sips), rest, gentle foods when tolerated, and careful use of medications. The key is knowing when it’s no longer “just a bug,” especially when dehydration, blood in stool, high fever, severe pain, or vulnerable health status enters the picture. When in doubtespecially for childrencall a healthcare professional early. It’s not overreacting; it’s preventing the “this got worse fast” sequel.