Table of Contents >> Show >> Hide
- First, Let’s Translate “Inoperable” into Plain English
- Challenge #1: Breathing Symptoms Turn Ordinary Days into Obstacle Courses
- Challenge #2: Treatment Can Feel Like a Part-Time Job (With No PTO)
- Challenge #3: Side Effects Often Stack, Not Separate
- Challenge #4: “Scanxiety” Is Realand It’s Not Just Nervousness
- Challenge #5: The Money Part Has a Name: Financial Toxicity
- Challenge #6: Stigma Shows Up at the Worst Possible Time
- Challenge #7: “Inoperable” Often Means the Goals of Care Need Frequent Re-Checking
- What Helps: A Two-Track Approach (Treat the Cancer, Treat the Person)
- What I Wish Every Family Asked at the Beginning
- Bonus: of Real-World Lessons (Composite Experiences)
- Conclusion
The word “inoperable” lands like a gavel. People hear it and assume the meeting is over, the options are gone, and the only thing left is to go home and stare dramatically out a window while it rains on cue.
But here’s the first lesson I wish everyone got on the same day as their diagnosis: inoperable does not mean untreatable. It often means surgery isn’t the right tool for this particular joblike trying to fix a leaky faucet with a chainsaw. The goal shifts (and sometimes expands) to controlling the cancer, easing symptoms, extending life, and protecting quality of lifeoften all at once.
Quick note before we begin: This article is educational, not medical advice. Lung cancer care is individualized, so decisions should always be made with an oncology team. Any “patient” examples below are composites drawn from common real-world themes.
First, Let’s Translate “Inoperable” into Plain English
“Inoperable” simply means the cancer can’t be treated with surgeryat least not safely, not completely, or not in a way that improves outcomes. Sometimes you’ll hear a related term: “unresectable”, meaning the tumor can’t be removed surgically.
In lung cancer, this can happen for a few big reasons:
- Location and extent: The tumor may involve structures where surgery would be risky or unlikely to remove all cancer.
- Stage and spread: Some cancers have spread within the chest (or beyond) in ways that make surgery an incomplete solution.
- Medical “inoperability”: A person’s heart or lung function (or other health conditions) may make surgery more dangerous than helpful.
One practical result: treatment often leans on systemic therapy (medicine that travels through the body, like chemotherapy, targeted therapy, or immunotherapy), radiation therapy, and supportive/palliative care. For certain stage III non-small cell lung cancers that can’t be removed, a common approach is chemotherapy combined with radiation (chemoradiation), sometimes followed by additional therapy such as immunotherapy to help keep the cancer stable.
Challenge #1: Breathing Symptoms Turn Ordinary Days into Obstacle Courses
If you’ve never been short of breath, you might imagine it’s “just” uncomfortable. People living with inoperable lung cancer teach you that breathlessness is also logistical. It affects how far you can walk, how you sleep, how you shower, whether you can climb stairs, and whether you can speak in full sentences without taking a break.
Common symptomslike a cough that won’t quit, chest discomfort, wheezing, hoarseness, fatigue, or shortness of breathcan pile up and make the world feel smaller. And when symptoms fluctuate, it’s easy to wonder, “Is this a bad day… or a sign of something bigger?” That uncertainty alone can be exhausting.
What I’ve learned is that symptom conversations work best when they’re specific. Not “I’m tired,” but:
“I’m winded after walking from the bedroom to the kitchen,” or
“I wake up coughing every night at 2 a.m.”
Those details help clinicians adjust treatment and supportive caresometimes quickly.
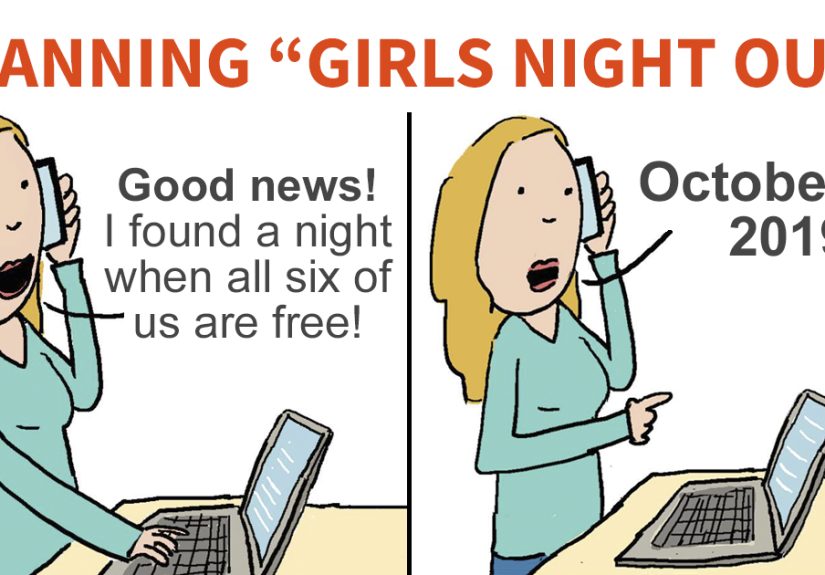
Challenge #2: Treatment Can Feel Like a Part-Time Job (With No PTO)
When surgery isn’t an option, care can become a carefully timed sequence: scans, lab work, infusions, radiation appointments, follow-ups, and side-effect management. It’s not just the treatmentit’s the infrastructure around treatment.
People often underestimate the invisible workload:
- Arranging rides (especially if you can’t drive afterward)
- Coordinating childcare or eldercare
- Tracking medications that change frequently
- Managing appetite, sleep, nausea, and fatigue
- Juggling insurance calls and prior authorizations (the hobby no one asked for)
One of the best coping strategies I’ve seen is building a “care operating system.” Not fancyjust reliable:
a single notebook or notes app for questions, symptoms, medication changes, and “what the doctor said when my brain temporarily left the building.”
Challenge #3: Side Effects Often Stack, Not Separate
People expect side effects to show up one at a time, like polite guests arriving at different hours. In reality, they tend to arrive like a group text that says, “We’re all here. 🙂”
Chemotherapy can cause fatigue, appetite changes, or increased susceptibility to infection. Radiation can create its own set of issues depending on the area treated. Immunotherapy can be incredibly effective for some people, but it also requires careful monitoring because it works by changing immune activity, which can sometimes inflame healthy tissue.
The lesson patients repeat (sometimes with impressive sarcasm) is: the goal is not “toughing it out.” The goal is getting through treatment with the fewest avoidable setbacks. That means reporting symptoms earlyespecially breathing changes, fevers, chest discomfort, severe fatigue, dehydration, or anything that feels like a sudden shift from your usual baseline.
Challenge #4: “Scanxiety” Is Realand It’s Not Just Nervousness
Scans are how oncology teams measure progress. For patients, scans are also how anxiety learns to use a calendar.
Many people feel a surge of dread before imaging, lab results, or big follow-up visitsoften called “scanxiety.”
What patients have taught me is that scanxiety isn’t solved by “just staying positive.” It’s helped by:
- Planning the waiting window: scheduling support, distractions, and small comforts for the 24–72 hours around results.
- Reducing uncertainty: asking when results will post, who will call, and what happens next in each possible scenario.
- Normalizing the reaction: naming it can reduce shame and make it easier to ask for help.
Humor helps too. I’ve heard more than one person say, “I’m not afraid of the scan. I’m afraid of the email that says, ‘Your results are available.’”
Honestly? Same.
Challenge #5: The Money Part Has a Name: Financial Toxicity
Cancer is a medical diagnosis that often turns into a financial crisis. Between deductibles, co-pays, travel, time off work, home support, and medications, costs can build quickly. There’s a term for this: financial toxicitythe harm that comes from the cost of care.
I’ve learned that many people wait too long to bring up cost concerns because they fear it sounds like they’re choosing money over life. But cost is part of access, and access is part of treatment. Practical steps that often help:
- Ask if your clinic has a financial navigator or social worker.
- Request generic or lower-cost alternatives when appropriate.
- Ask about assistance programs through hospitals, nonprofits, or drug manufacturers.
- Discuss work accommodations and disability paperwork earlybefore exhaustion makes it harder.
The most important lesson: you are not “being difficult” by asking about costs. You’re being realistic.
Challenge #6: Stigma Shows Up at the Worst Possible Time
Lung cancer carries a particular kind of stigmaoften wrapped up in the question, “Did you smoke?” Even when the answer is “no,” the question can feel like an accusation instead of curiosity.
What patients teach us is that stigma steals energy that should be used for healing. It can also make people hesitate to seek support, tell employers, or even share their diagnosis with friends.
The truth is simple: anyone with lungs can get lung cancer. Smoking is a major risk factor, but it’s not the only one; secondhand smoke, radon exposure, air pollution, and workplace exposures can also contribute. Support is not something people should have to “earn” by passing a moral quiz.
Challenge #7: “Inoperable” Often Means the Goals of Care Need Frequent Re-Checking
One of the hardest parts of inoperable lung cancer is that the goalposts can move. The goal might be to:
- Shrink or control the cancer
- Prevent progression
- Relieve symptoms
- Buy time for a better therapy (or a clinical trial)
- Protect daily functioning and comfort
Patients do best when everyone agrees on the current goaland revisits it regularly. This is not “giving up.” It’s good strategy.
A helpful question is:
“What are we trying to achieve with this next stepand how will we know if it’s working?”
What Helps: A Two-Track Approach (Treat the Cancer, Treat the Person)
Inoperable lung cancer care works best when it runs on two tracks at the same time:
cancer-directed treatment plus symptom/supportive care.
People sometimes hear “palliative care” and think it means end-of-life care only. In reality, palliative care can be layered in early to improve quality of life, manage symptoms, and support decision-makingwhile cancer treatment continues.
Supportive care can include:
- Breathlessness strategies and pulmonary support
- Pain management and sleep support
- Nutritional counseling when appetite is low
- Help for anxiety and depression (because this is a lot)
- Procedures that relieve symptoms, like draining fluid buildup or opening a blocked airway when needed
Patients often describe this as “getting my life back in the middle of treatment.” That’s not a small winthat’s the point.
What I Wish Every Family Asked at the Beginning
The best questions are simple, specific, and repeatable:
- What type of lung cancer is this (NSCLC vs SCLC), and what stage?
- Is it inoperable because of location/stage, or because surgery is too risky for me medically?
- Has my tumor been tested for biomarkers that might open targeted therapy options?
- What is the goal of treatment right now: control, shrinkage, stability, symptom relief?
- What side effects should trigger a same-day call?
- Do you recommend palliative care alongside treatment?
- Are there clinical trials I should consider?
If you can bring one person to appointments (in person or on speakerphone), do it. Not because you “can’t handle it,” but because no one should have to remember complex medical details while emotionally processing life-changing news.
Bonus: of Real-World Lessons (Composite Experiences)
Over and over, people with inoperable lung cancer teach the same surprising truth: the hardest part isn’t always the cancer. It’s the constant adapting.
One person (a composite of many stories) described life as “living between appointments.” The calendar became the boss. Mondays were labs. Tuesdays were radiation. Thursdays were infusion. Fridays were recovery. Weekends were for trying to feel like a person againplus laundry, because cancer is rude and still expects clean socks.
The lesson: protect your “non-cancer hours.” Schedule something small that’s yoursan audiobook chapter, a short walk, a favorite show, a call with a friend who can talk about literally anything else. These aren’t distractions; they’re oxygen for the mind.
Another person told me the most stressful moment wasn’t treatment dayit was the three days waiting for scan results. They called it “the doom gap.” They weren’t crying nonstop; they were functional. But their thoughts ran in the background like an app draining battery life.
The lesson: make the waiting plan as real as the treatment plan. Ask, “When will results post? Who explains them? If it’s good news, what’s next? If it’s not, what’s next?” A clear workflow doesn’t erase fear, but it reduces the feeling of free-falling.
I also remember a caregiver who said, “Everyone asked how my spouse was doing. No one asked how I was doing.”
Caregivers are often running logistics, managing meds, cleaning, cooking, driving, and quietly absorbing fear like a sponge that never gets wrung out.
The lesson: caregivers need care plans too. That might mean a rotating meal calendar, a ride schedule, a respite day, or a support group. If you’re the patient, “accepting help” isn’t being needyit’s letting your team stay strong for the long haul.
Then there’s the emotional curveball of stigma. A patient who never smoked described feeling like they had to “prove” they deserved sympathy. Another patient who used to smoke felt judged in a way that shut down conversation.
The lesson: replace blame with useful questions. “How can I help?” beats “How did this happen?” every time. And for patients: you don’t owe anyone your risk-factor résumé. Your diagnosis is not a morality play.
Finally, I’ve learned that people want honesty without hopelessness. They don’t want false cheerleading, but they also don’t want to be treated like a statistic.
The best care teamsand the most resilient patientsmake room for both: grief and planning, fear and humor, realism and hope.
The lesson: hope is allowed to be practical. Sometimes hope is a new therapy. Sometimes it’s a stable scan. Sometimes it’s making it to a graduation, a birthday, or just a Tuesday that feels calm.
Inoperable lung cancer can be brutally hard, but patients showagain and againthat life can still contain meaning, connection, laughter, and choice.
Conclusion
Inoperable lung cancer brings real challenges: symptoms that disrupt daily life, treatment schedules that demand stamina, emotional stress that spikes around scans, financial strain, and stigma that no one needs.
And yet, patients also show what works: clear goals, honest communication, early symptom support, practical planning, and community.
If there’s one takeaway I’d put in bold, underline, and maybe tattoo on the healthcare system (in washable ink): “Inoperable” is not the end of the conversationit’s the beginning of a different strategy.